Surgical Innovation: Valve Wrapping Techniques Used During The Ross Procedure With Dr. Paul Stelzer
By Adam Pick on August 24, 2012
I’ll never forget my 3-week check-up when Dr. Starnes, my heart surgeon, said to me, “Adam, the post-operative echocardiogram shows that your heart is doing excellent… Plus, we wrapped your pulmonary valve during the procedure, so you should benefit from that over time.” In the moment, I didn’t question Dr. Starnes about my wrapped pulmonary valve. To be honest, I didn’t care. I just wanted to hear that my heart was doing well after my double heart valve replacement surgery.
However, as the community at HeartValveSurgery.com grew, I received several patient questions about “valve wrapping techniques” used during the Ross Procedure, a unique form or aortic valve replacement surgery. For that reason, I contacted Dr. Paul Stelzer, a Ross Procedure specialist at Mount Sinai Medical Center, to discuss this surgical innovation.
In our exchange, I asked Dr. Paul Stelzer, MD three questions:
- What is a valve wrapping technique?
- Why is it done?
- Does it produce a better surgical result?
Below, you will find an incredibly detailed response from Dr. Stelzer. Please note, however, Dr. Stelzer’s comments are technical and loaded with several research references.
Dr. Stelzer’s Comments About Valve Wrapping Techniques For The Ross Procedure
I have been asked to comment on “wrapping” techniques for the Ross Procedure. Having lived through the evolution of technique for over 25 years, I have learned a lot about the behavior of the pulmonary autograft when put into the high pressure aortic environment. It took many years of observation to obtain clinical and microscopic evidence of what actually happens. Dilatation of the root was what we saw 10-15 years after surgery. We now know that the leaflets of the valve can and do change their architecture to increase the amount of elastic fibers and align the cells in a way that will make the leaflets stronger. (See elegant pathologic study by Rabkin-Aikawa et al – 2004.)
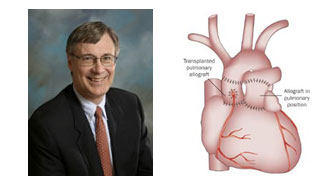
Dr. Paul Stelzer – Ross Procedure Specialist
An initial deposition of collagen protein on the underside of the leaflets holds them together while this transformation takes place but then is largely absorbed when it is no longer needed. The pulmonary arterial wall, however, responds to the higher aortic pressure by layering itself with collagen that does not go away and the intrinsic elastic fibers are fragmented never to return to their normal function.
This results in maximal expansion of the pulmonary root that never contracts or regains its elasticity as a neo-aortic root. A slow dilatation is usually seen and the unsupported autograft root can reach sizes over 7 cm in diameter. Many of these have been replaced on the basis of echo or CT scan measurements that raise concern about dissection or rupture possibilities. From a practical standpoint, we know that most roots will not dilate up to dangerous aneurysms and rupture has never been reported. Localized dissection has been seen but is prevented from propagating into the native aorta, the valve or the coronaries by the suture lines placed at the time of the original surgery.
The primary consequence of the dilatation has been aortic regurgitation which is, of course, undesirable with volume load on the left ventricle and ultimately need for repair or replacement of this valve. Some can be repaired with valve-sparing root reconstruction but many have to be replaced.
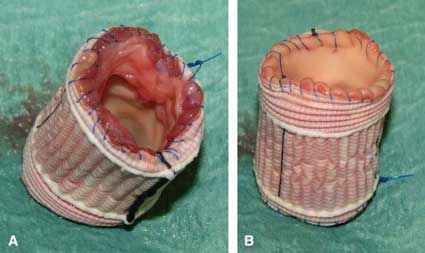
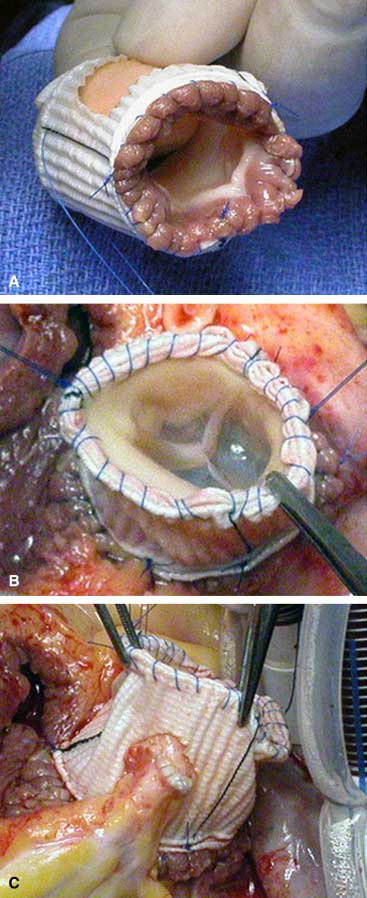
Wrapping the autograft root in various ways has been used with the intent of limiting the expansion of the tissue so that the valve will remain competent and the root will not become an aneurysm over time. Materials such as pericardium, Gortex and Dacron graft have been employed. The native aortic root tissue has also been used including the use of the original Donald Ross “subcoronary” technique (Hans Sievers), the “root inclusion” technique (Peter Skillington), or the “native jacket” method that I prefer.
Enclosing the autograft root completely in a tube of Gortex, Dacron, or pericardium is effective but can easily be overdone to the point of distorting the leaflets and causing the very regurgitation we want to prevent. The key points of support are the annulus (inflow end) and the sinotubular junction (outflow end) of the crown-shaped leaflet insertion line. This is easily done with a strip of Teflon felt or pericardium – the point being to use a material that will not stretch over time and to make it just the right length to maintain the original dimensions of the autograft.
Tirone David has pointed out that dilatation of the sinuses of Valsalva has no impact on the function of the aortic valve. They look scary on imaging but don’t really cause trouble. We can accomplish both good function and good looking echo pictures by judiciously including the native elements of the aortic wall around the autograft root. If the native aortic root is already very dilated, they won’t help much on their own so an extra layer of prosthetic material such as Dacron or Gortex adds a layer of strength. If these are left open around the coronary “buttons” there is a little radial distensibility to the root that is more like the original machinery.
The bottom line is that we want the pulmonary autograft root to adapt and behave as much like a normal aortic root as possible for the best long term result. Use of the original “subcoronary” technique can accomplish this but is technically more difficult to achieve and frequently requires “tailoring” the aortic root to match the autograft properly. Some patients are eliminated from the operation because of their coronary anatomy which is rarely a problem with the root replacement method. The “root inclusion” has been very successful in Skillington’s hands but is also more technically challenging with more potential for compromise of the coronary arteries. The routine “re-inclusion” of native aortic root tissue around the autograft as a full root replacement (with proximal and distal strips of felt) is probably the most widely applicable and reproducible method.
The German-Dutch Ross registry data (Charitos et al – 2009) demonstrate the durability advantage of the double-ended root support is equal to the subcoronary technique and superior to the unsupported root at the ten year point post-op. When to add further material outside of the sinuses is a matter of surgical judgment but is most likely wise in the patient with a root/ascending aneurysm and primary aortic regurgitation with a bicuspid valve. It took us over a decade of experience to see enough long term follow up to realize what can happen to the autograft over time.
Armed with that information, we can now use appropriate support techniques that I believe will extend the feasibility of the operation to more patients and extend its durability to all.
Adam’s Response To Dr. Stelzer’s Comments
All I can say is “Wow!”
I’m not sure I understood everything that Dr. Stelzer discussed… But, I think I now understand the main benefits of pulmonary (autograft) valve wrapping during the Ross Procedure. It appears this surgical innovation helps:
- Preserve the function of the pulmonary valve which has been shifted to the aortic position;
- Protect against the possibility of aortic regurgitation;
- Provide added support to minimize the risk of aortic root dilation; and
- Minimize the possibility of an aortic aneurysm forming.
As always, thanks so much to Dr. Paul Stelzer for sharing his clinical experiences and research with our patient community. These comments were very, very, very helpful. To learn more about Dr. Stelzer, click here.
Keep on tickin!
Adam
|
Naomi says on September 7th, 2012 at 10:55 am |
|
Your ideas and procedures are very interesting. I am a young student and I would like to be a cardiovascular surgeon when I am older. Although I don’t quite understand many things you talk about in your blog, I look forward to researching more about a “Ross Procedure.” Thank you for the inspiration! |
 |