Surgeon Insights: The Different “Faces” of Mitral Valve Disease
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Dr. Marc Gerdisch, Chief of Cardiac Surgery at Franciscan Health
Published: June 11, 2023
Mitral valve disease is super complex. From malformed leaflets to annular calcification to endocarditis, there are many different types of mitral valve disorders. For this reason, it is critical that patients understand their specific type of mitral valve disease and the therapies that yield the best, long-term outcomes.
To explore the different types, or “faces”, of mitral valve disease, we sat down with Dr. Marc Gerdisch, the Chief of Cardiac Surgery at Franciscan Health in Indianapolis, Indiana. Dr. Gerdisch is a mitral valve expert who has performed over 5,000 heart valve procedures and successfully treated more than 100 patients in our community. It was fascinating to hear Dr. Gerdisch describe the different mitral valve faces that he sees in the operating room.
Key Learnings About The Different Faces of Mitral Valve Disease
The key learnings from Dr. Gerdisch about the different faces of mitral valve disease include:
- A common face of mitral valve disease is mitral insufficiency, also known as mitral regurgitation. “Probably the thing that gets talked about the most is mitral insufficiency, leaking mitral valve,” states Dr. Gerdisch. “It’s really the prize of mitral valve surgery in the sense in that nearly 100 percent of those patients will be repaired and will be restored to a normally functioning valve.”
- A complex face of mitral valve disease may include mixed regurgitation with calcification. According to Dr. Gerdisch, “There are also patients that make up a large swathe outside of standard myxomatous degenerative leaking valves that have either mixed disease, meaning that they have myxomatous disease, that’s classic, degenerative, billowy valves, soft leaflets but they also have, for example, calcification of the valve or they have changes in the architecture of the valve beyond those changes.”
- A “rising face” of mitral valve disease is extensive calcification from Rheumatic fever. Dr. Gerdisch states, “We see more and more patients that have extensive calcification of the mitral valve… As a result of that, the leaflets become thick, immobile. Blocked mitral valves have always been the focus there. If we look worldwide, rheumatic mitral valve disease is still the most common mitral valve disorder. What I’m trying to get at is that someone can have an echocardiogram, it can say the valve is leaking but that doesn’t mean that it’s a myxomatous degenerative valve. You can have a rheumatic mitral valve that leaks and isn’t obstructed but it’s a function of the leaflets not moving enough, not getting together, not closing properly.”
- Another rising face of mitral valve disease is overlapping valve leaflets. “Changes in what we call coaptation, where the leaflets overlap, can be a function of the leaflets being too free to move, so that’s myxomatous degenerative disease. It could be that the leaflets can’t move, and they can’t reach each other, so you don’t have that overlap and that can be the problem. Now, let me give you both. Now, you’ve got one leaflet that moves too much and you’ve got another leaflet that doesn’t move enough.”
- Secondary mitral valve disease presents a different face of mitral valve disease. According to Dr. Gerdisch, “The other category that I think really mystifies patients, that they can’t really get full information on because it’s difficult to understand is the general concept of secondary mitral valve disease, mitral insufficiency driven by other conditions – dilated lower chamber, hypertension, coronary artery disease.”
- Endocarditis infections are another rising face of mitral valve disease. “Among the spectrum of disorders, the faces of mitral disease, I did mention endocarditis. Any valve can be infected, and we still strive to reconstruct that valve. Often, we can use whatever tissue is left after whatever destruction has been done by the infection, patch the area that we have to clean out from the infection, reconstruct the valve and then we still re-support it with a valve ring,” according to Dr. Gerdisch.
- Hypertrophic Cardiomyopathy is another rising face of mitral valve disease. “Other conditions, for example hypertrophic cardiomyopathy. That’s a mouthful but it is basically when people have a very thick heart and then part of that very thick heart obstructs the blood flow getting out of the left ventricle out to the body,” states Dr. Gerdisch. “The blood accelerates as it leaves the ventricle. It’s passing by the mitral valve on its way out and the high-velocity jet will actually grab on to the anterior leaflet of the mitral valve and it gets stuck down there. Now, you’ve got to fix that, of course.”
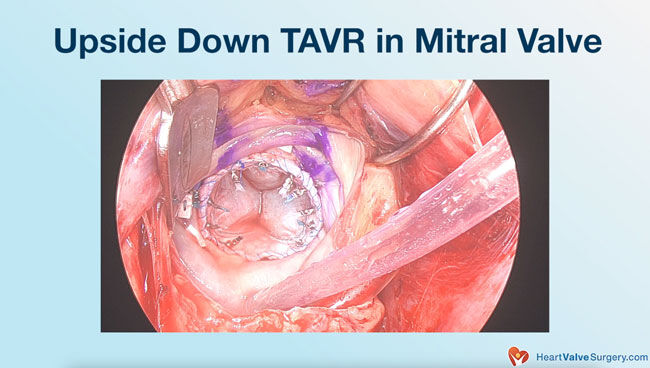
- Dr. Gerdisch will use advanced surgical techniques to address the different faces of mitral valve disease which may include an upside down TAVR in the mitral valve.
- The goal of treating mitral valve disease is to repair the valve whenever possible. According to Dr. Gerdisch, “When we’re approaching a mitral valve that’s complex, we have to orchestrate our thought process around everything about the patient and what we’re doing. It never is one size fits all. When we see varying morphology or changes in the valve, we sometimes have to become creative about how we’re going to go about their repair. It might also move us away from, for example, a minimally invasive repair to doing a sternotomy approach, especially since we do rigid fixation for all the sternotomies. We can give them back their mobility quickly and still repair the valve.”
- Using minimally-invasive techniques should not sacrifice the possibility of a mitral valve repair. Dr. Gerdisch states, “The other thing you’ve heard me say before is that we never sacrifice a perfect repair for a small incision. We get into the more exotic repairs, we’re taking calcium out, we’re changing more of the architecture of the valve, then we might think of moving over to a larger exposure just because we know that we’re going to get the job done.”
- Dr. Gerdisch advises mitral valve disease patients is to understand their specific type of mitral valve disease, the condition of the heart, and the treatment options available to them. “My recommendation for the patient is first, any abnormality of any echocardiogram has to be explained and then any change has to be explained,” states Dr. Gerdisch. “We really need to become intimate with that, with respect to what it means to the particular patient. The patient has to seek that information from their cardiologist and from their heart surgeon. They have to have a conversation, a dialog.”
Many Thanks to Dr. Gerdisch & Franciscan Health!!
On behalf of our entire patient community, many thanks to Dr. Gerdisch for sharing his clinical experiences and research with our community! Also, many thanks to the Franciscan Health team for taking such great care of heart valve patients.
Related links:
- Surgeon Insights: Minimally-Invasive Mitral Valve Repair Surgery
- Top 5 Facts About Dr. Gerdisch’s Rapid Recovery Protocol
- See 100+ Patient Reviews for Dr. Gerdisch
Keep on tickin!
Adam
P.S. For the hearing impaired members of our community, I have provided a written transcript of the video with Dr. Gerdisch below.
Video Transcript:
My name is Marc Gerdisch. I am chief of cardiothoracic surgery at Franciscan Health in Indianapolis, Indiana.
I do think a good way of putting it is the different faces of mitral valve disease. In the context of just saying a valve leaks or it’s blocked, you don’t really understand the organic changes that are involved in the valve and how they relate to the rest of the heart and what the expectations should be for the patient and what can be done for it.
A Common Face of Mitral Valve Disease: Mitral Insufficiency
Probably the thing that gets talked about the most is mitral insufficiency, leaking mitral valve.
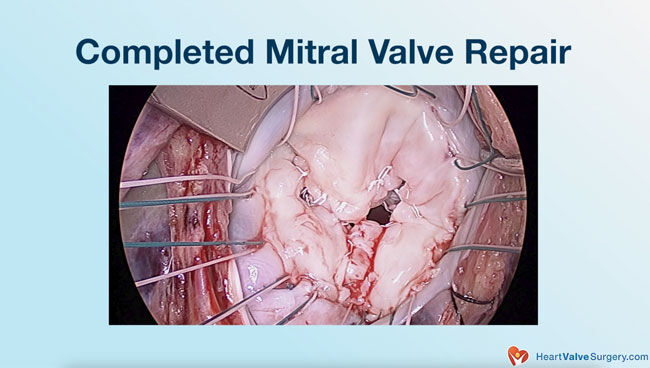
It’s really the prize of mitral valve surgery in the sense in that nearly 100 per cent of those patients will be repaired and will be restored to a normally functioning valve.
We can do it minimally invasively. We have patient recovery that’s great and the whole process is pretty well established, step by step.
A Complex Face of Mitral Valve Disease: Mixed Regurgitation with Calcification
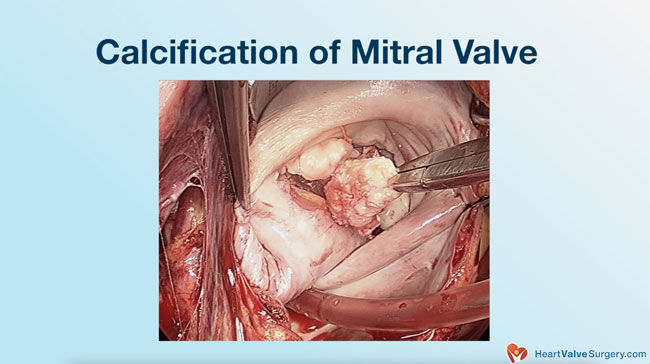
There are also patients that make up a large swathe outside of standard myxomatous degenerative leaking valves that have either mixed disease, meaning that they have myxomatous disease, that’s classic, degenerative, billowy valves, soft leaflets but they also have, for example, calcification of the valve or they have changes in the architecture of the valve beyond those changes. Those are mixed changes.
For example, someone can have myxomatous degenerative disease but also have changes in the shape of their heart that would give them what we call, functional mitral regurgitation. It results due to changes in geometry of the heart. It pulls down on the valve, it changes the position of the leaflets. It changes your ability to repair it or to get a long durable repair. The assessment of those patients becomes more complicated.
Rising Faces of Mitral Valve Disease: Extensive Calcification from Rheumatic Fever
In addition, now we see more and more patients that have extensive calcification of the mitral valve. There are probably a couple of reasons we’re seeing it more. Number one is because we’re paying more attention. Number two is because people are living longer and as you age, you’re at greater risk of calcification, especially around the valve in what we call the anulus or the place where the leaflets attach. It’s becoming more of a disease entity.
In the past, leaflets not moving well or obstruction to the valve was largely described in the realm of rheumatic disease. We still see rheumatic disease, especially in areas that are rural where people maybe don’t see the doctor as much. In their early life, they could have a strep throat and not have it treated and that’s what leads then to rheumatic fever. Rheumatic fever leads to rheumatic valve disease because the patients develop antibodies to their own body, to their own valve. As a result of that, the leaflets become thick, immobile. Blocked mitral valves have always been the focus there. If we look worldwide, rheumatic mitral valve disease is still the most common mitral valve disorder.
What I’m trying to get at, though, is that someone can have an echocardiogram, it can say the valve is leaking but that doesn’t mean that it’s a myxomatous degenerative valve. You can have a rheumatic mitral valve that leaks and isn’t obstructed but it’s a function of the leaflets not moving enough, not getting together, not closing properly.
Rising Faces of Mitral Valve Disease: Overlapping Valve Leaflets (Coaptation)
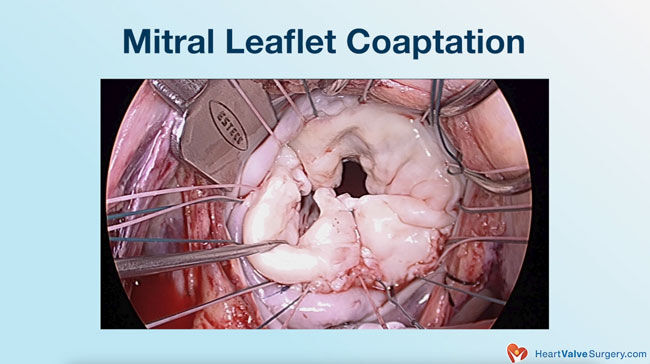
Changes in what we call coaptation, where the leaflets overlap, can be a function of the leaflets being too free to move, so that’s myxomatous degenerative disease where the leaflet goes like this, and the blood comes up from the ventricle into the atrium. It could be that the leaflets can’t move, and they can’t reach each other, so you don’t have that overlap and that can be the problem. Now, let me give you both. Now, you’ve got one leaflet that moves too much,
you’ve got another leaflet that doesn’t move enough and can that be remedied? Sometimes, we’re going to bring this leaflet down and then we might expand this leaflet to make it bigger so that we can have that relationship re-established.
Different Faces of Mitral Valve Disease: Secondary Mitral Valve Disease
Again, many faces of mitral valve disease. The other category that I think really mystifies patients, that they can’t really get full information on because it’s difficult to understand is the general concept of secondary mitral valve disease, mitral insufficiency driven by other conditions. For example, I talked earlier, change in the shape of the ventricle leading to a leaking valve. Those are people who, for some reason, the lower chamber of the heart has enlarged; it’s dilated. Now that can just happen to people; they get idiopathic myopathy. It can be driven by comorbid conditions like hypertension. It can be a function of coronary artery disease, injury to the heart and change in the shape. Then they go on to have a leaking mitral valve.
Rising Faces of Mitral Valve Disease: Endocarditis Infection
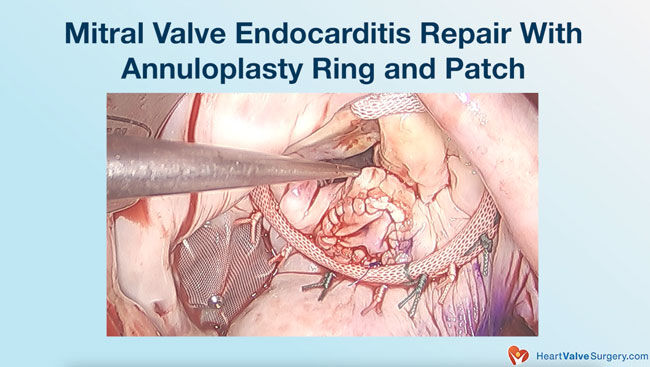
Among the spectrum of disorders, the faces of mitral disease, I did mention endocarditis. Any valve can be infected, and we still strive to reconstruct that valve. Often, we can use whatever tissue is left after whatever destruction has been done by the infection, patch the area that we have to clean out from the infection, reconstruct the valve and then we still re-support it with a valve ring.
People are very familiar with that for valve repair. I think it’s important to recognize that any time that you have a moderate amount of normal tissue still present in the valve, the goal is going to be to integrate that into a repair and save the valve. That includes infection, when you have leaflet or tissue around the valve that’s destroyed.
Rising Faces of Mitral Valve Disease: Hypertrophic Cardiomyopathy
Other conditions, for example hypertrophic cardiomyopathy. That’s a mouthful but it is basically when people have a very thick heart and then part of that very thick heart obstructs the blood flow getting out of the left ventricle out to the body. The blood accelerates as it leaves the ventricle. It’s passing by the mitral valve on its way out and the high-velocity jet will actually grab on to the anterior leaflet of the mitral valve and it gets stuck down there. Now, you’ve got to fix that, of course. Sometimes, it’s just taking the muscle out, changing the muscle architecture, sometimes, you repair the valve. There will be instances where that has been like that so long that the anterior leaflet has literally become beaten up and doesn’t function well anymore.
Different Faces of Mitral Valve Disease: Advanced Surgical Techniques
Depending on the patient’s overall physiology, what the opportunity looks like, how old they are, what other conditions they have, we may become very aggressive about taking that calcium out and then rebuilding the valve so that we give them a repaired valve.
In someone else, let’s say perhaps an older person, after about 80-82 years of age, we don’t see a survival benefit for those people. We have science that tells us when we’re supposed to be very aggressive or do what I would call an exotic repair. If the patient is best served with a replacement, our goal would be to not disturb the anatomy as much as possible. We avoid disrupting the anatomy but then replace the valve with a generously sized tissue valve in an older person. Still, we do anything we can to not change the geometry of the heart.
If, for example, a valve has to be replaced and you cut out a leaflet or both leaflets or some of the leaflet tissue. Now, the connections between those leaflets and the ventricle, the chamber, which is normally shaped like this are severed. It’s like an upside-down ice cream cone because that’s how the muscle is. When the heart squeezes, it spirals and pushes the blood out. Now, if I cut the connection to the papillary muscles here and they drop down, the heart changes shape. It’s really important that if the valve has to be replaced that everything possible is done to maintain that relationship. We will literally reconnect those papillary muscles in some fashion, up to the upper portion of the heart so that the shape is maintained.
Across the spectrum of all these different faces of mitral disease, still repair remains our goal because we know that once we – I’ve often said this and people quote me sometimes that when we change the valve, we’re trading diseases.
Once you implant a prosthetic valve, you’ve changed the really bad disease the patient has for a lesser disease where they now have a prosthetic valve that they have to deal with either the continuous blood thinner or the degeneration, deterioration of a valve. The impact of that is different for different people, based on their comorbidities and age.
When we’re approaching a mitral valve that’s complex, we have to orchestrate our thought process around everything about the patient and what we’re doing. It never is one size fits all. When we see varying morphology or changes in the valve, we sometimes have to become creative about how we’re going to go about their repair. It might also move us away from, for example, a minimally invasive repair to doing a sternotomy approach, especially since we do rigid fixation for all the sternotomies. We can give them back their mobility quickly and still repair the valve.
Different Faces of Mitral Valve Disease: Minimally-Invasive Considerations
The other thing you’ve heard me say before is that we never sacrifice a perfect repair for a small incision. We get into the more exotic repairs, we’re taking calcium out, we’re changing more of the architecture of the valve, then we might think of moving over to a larger exposure just because we know that we’re going to get the job done.
It’s always a process that requires real intent to design what you’re going to do to the valve. There are cases where, for example someone who’s very old or very debilitated where we will even take a transcatheter aortic valve, flip it upside down and put it inside of the native valve. There are transcatheter scenarios, even through the leg, placing a transcatheter valve in a calcified doughnut of a mitral valve. You can also do it surgically if needed; take out one leaflet, implant that upside down transcatheter valve.
Now, there are technologies that they’re working on, of course that are pipeline, that are going to be completely percutaneous mitral valves. It’s still going to be extremely difficult to treat these patients because of the circumferential calcification and the limitations of the space in there. We always have to finish up, hopefully, with a big valve.
Different Faces of Mitral Valve Disease: Surgeon Recommendations for Patients
My recommendation for the patient is first, any abnormality of any echocardiogram has to be explained and then any change has to be explained. I think, for example, people have atrial fibrillation and it may or may not be adequately managed but they aren’t at a point where they’re having surgery for something. That atrial fibrillation has been ongoing for so long that the atria get big and then the valves start to leak, and it can be the mitral valve leaking. Looking at the spectrum of that patient’s life, how they live their life, what their longevity is like, what their expectations are, when do you decide to intervene for something like that? Is the moderately leaking mitral valve and moderately leaking tricuspid valve, along with the continuous atrial fibrillation and enlarging atria enough to do something. It might be for some people. Other people, it’s when it’s severe. The point is that something as benign as atrial fibrillation can lead to valve problems.
When we see mild to moderate insufficiency, changes in the shape of the heart, changes in strain or the dimensions of the chambers, we really need to become intimate with that, with respect to what it means to the particular patient. The patient has to seek that information from their cardiologist and from their heart surgeon. They have to have a conversation, a dialog.




