Medical Breakthrough: New Radiopaque Markers On Epic Plus Valve
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: Jason Rogers, MD, Clinical Professor of Cardiovascular Medicine and the Director of Interventional Cardiology at UC Davis Health
Published: September 14, 2022; This post is sponsored by Abbott.
The innovation within next-generation heart valve replacement devices is downright fascinating. As a result, patients may benefit from minimally-invasive techniques, better durability, shorter hospital stays, and now… Valve-in-Valve reoperations.
For example, we are just learning about the use of radiopaque markers on the new Epic Plus Valve that recently received FDA approval. To learn how radiopaque markers help interventional cardiologists use non-invasive devices during Valve-in-Valve procedures, we interviewed Dr. Jason Rogers, the Clinical Professor of Cardiovascular Medicine and the Director of Interventional Cardiology at UC Davis Health in Sacramento, California.
Key Learnings About Radiopaque Markers & Valve-in-Valve Devices
Here are several important points to consider from our interview with Dr. Rogers:
- Dr. Rogers is an interventional cardiologist. An interventional cardiologist is a cardiologist who specializes in procedures to fix the heart, either the arteries or the valves, using small catheters, or tubes, via non-invasive techniques under fluoroscopy (x-ray). Interventional cardiologists are not cardiac surgeons and do not perform “open-heart surgery” using incisions to the patient’s chest or ribs.
- Heart valve reoperations are required when tissue or mechanical valve replacements fail. In the past, failing valve replacements were re-replaced during open-heart surgery. Today, Valve-in-Valve procedures enable interventional cardiologists, cardiac surgeons and heart teams to use non-invasive, transcatheter devices to replace failing tissue valves without open-heart surgery.
- According to Dr. Rogers, there are between 3,000 to 4,000 mitral valve reoperations performed annually in the United States. Dr. Rogers states, “Reoperation for recurring mitral valve disease is not uncommon.”
- Dr. Rogers believes this new approach for tissue valve reoperations, using Valve-in-Valve devices, is a game changer considering patient benefits. “This is a game changer,” states Dr. Rogers. “This is a way to replace a tissue valve a second time without a conventional surgical incision. We are not opening the patient up. We can do this quickly through a small tube in the leg. We do it under general anesthesia so the patients are comfortable, and they can go home the next day with a new functioning valve.”
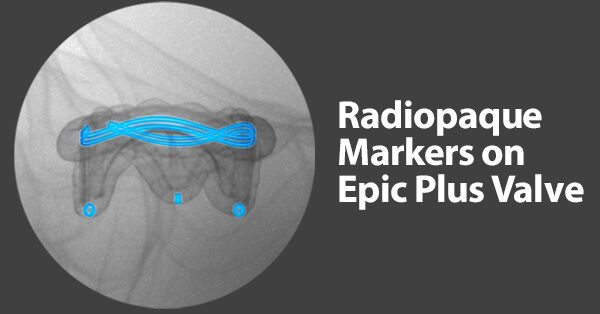
- Radiopaque markers are used to help interventional cardiologists and surgeons position a Valve-in-Valve device. Dr. Rogers states, “There are some new valves, such as the Epic Plus valve, that have unique x-ray markers that allow us to position the new valve in there, and also has a lower profile that may limit any obstruction that the new valve will cost.”
- Considering the opportunity provided by the Epic Plus surgical valve for a Valve-in-Valve procedure in the future, this unique valve offers a new approach for the lifetime management of heart valve disease. “Yes, we have a lot of innovation and improvements that allow a lifetime management for these patients,” states Dr. Rogers.
- The use of x-ray guidance and radiopaque markers are very important during a Valve-in-Valve procedure. “We use x-ray to guide these procedures. We can actually see the frame of the surgical valve on x-ray. It usually has a dark appearance. Then we can use that to position our new valve inside. The new valve gets inflated on a balloon and it will actually insert inside the old surgical valve. We put a new, fresh, functioning valve inside of the prior valve.”
Many Thanks to Dr. Jason Rogers & Abbott
On behalf of the patients at HeartValveSurgery.com, many thanks to Dr. Jason Rogers for sharing his clinical experiences and research with our community. We would also like to thank Abbott, the company which manufactures the Epic Valve for their dedication and commitment to helping patients with heart valve disease.
Related Links:
- Epic Plus Gets FDA Approval for Lifetime Management of Heart Valve Disease
- Doctor Q&A: Biological Heart Valve Replacement Durability
- Robotic Mitral Valve Replacement: What Should Patients Know?
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our patient community, I have provided a written transcript of this video below.
Video Transcript:
Adam: Hi, everybody. It’s Adam with HeartValveSurgery.com, and today we have a very special cardiologist question and answer session all about the innovation in mitral valve reoperations. I am thrilled to be joined by Dr. Jason Rogers, who’s a leading interventional cardiologist at UC Davis in Sacramento, California. Dr. Rogers, it is great to see you again. Thanks for being with us today.
Dr. Jason Rogers: Great to be here, Adam, with the HeartValveSurgery.com audience and to see you again.
Adam: Yeah, and we’re going to be talking all about your specialty in mitral valve reoperations and some of the innovations you’re working on, but first, to help educate the patients, can you share with them, what is an interventional cardiologist?
Dr. Jason Rogers: Great question, Adam. An interventional cardiologist is a cardiologist who specifically specializes in doing procedures to fix the heart, either the arteries or even the valves, using small catheters or tubes, and not having to do conventional heart surgery with say a scalpel.
Adam: Dr. Rogers, it’s great to hear what you’re doing there with these noninvasive approaches. Now let’s really dig into it. When it comes to the mitral valve and reoperations of the mitral valve, can you share with our community about any trends in that procedure? Is this something that’s increasing or decreasing?
Dr. Jason Rogers: That’s actually quite interesting, Adam. There’s about 3,000 to 4,000 patients a year in the US who are undergoing another cardiac operation on the mitral valve. These are patients who’ve had mitral valve surgery once before in their lives and are having it again. Reoperation for mitral valve is not uncommon.
Adam: Dr. Rogers, I didn’t know the number of reoperations was so high. I’m curious to know, how are you as an interventional cardiologist helping patients who may need a mitral valve reoperation?
Dr. Jason Rogers: Great question. As always, we work as a team with cardiologists and surgeons to decide what’s best. Many patients who need a second operation are at higher risk for conventional surgery. They’ve already had one operation. One therapy we can offer for some patients is what’s called valve-in-valve. We actually insert a new catheter valve through a small tube in the leg, into the old surgical valve and essentially refresh it, giving it a new function and making it work like new.
Adam: Dr. Rogers, this sounds like a fascinating procedure. I’m curious to know, in the world of valve therapy, would this fall into a category of let’s say a game changer?
Dr. Jason Rogers: Absolutely, this is a game changer. This is a way to replace the valve a second time without a conventional surgical incision. We are not opening the patient up. We can do this quickly through a small tube in the leg. We do it under general anesthesia so the patients are comfortable, and they can go home the next day with a new functioning valve.
Adam: Dr. Rogers, I love hearing about all the patient benefits. I’m curious to know, have there been any innovations in valve therapies or devices that have given you this opportunity? If so, is it important for your surgical team to consider those?
Dr. Jason Rogers: Adam, absolutely. We are looking at a lifetime management strategy for patients with surgical mitral valve replacement. We know no valve will last forever, and we have to consider what we will do down the line. Issues such as valve diameter, the correct size, having it be large enough for a valve-in-valve therapy in the future are important. There are some new valves, such as the Epic Plus valve, that have unique x-ray markers that allow us to position the new valve in there, and also has a lower profile that may limit any obstruction that the new valve will cost. Yes, we have a lot of innovation and improvements that allow a lifetime management for these patients.
Adam: Dr. Rogers, this is amazing. Can you talk about those markers and how you use them during valve-in-valve therapies?
Dr. Jason Rogers: We use x-ray to guide these procedures. We can actually see the frame of the surgical valve on x-ray. It usually has a dark appearance. Then we can use that to position our new valve inside. The new valve gets inflated on a balloon, as you can see, and it will actually insert inside the old surgical valve. We put a new, fresh, functioning valve inside of the prior valve.
Adam: Dr. Rogers, are there any innovations for this new Epic Plus valve specific to durability?
Dr. Jason Rogers: There are constantly new innovations in terms of the way that these valves are prepared, the way the leaflets are preserved, like the Linx AC technology. The bottom line though is that all surgical valves have a lifespan, and at some point the patients will need a repeat operation. We really need to be thinking down the road what is going to be the option for a given patient.
Adam: Dr. Rogers, if I’m a patient and I need a first mitral valve replacement, what consideration should I have as I go through this process?
Dr. Jason Rogers: Adam, it’s very natural for the patient and the surgeon to be very focused on that initial operation and a lot of the logistics, how long will I be in the hospital, how long will it take me to recover. One thing we don’t often discuss enough is what is going to be the management down the line for that patient’s lifetime. I think my advice to patients would be to understand the procedure you’re having now, but ask your surgeon and your cardiologist, hey, what’s the plan going to be 7 to 10 years down the line when I need a new valve? Perhaps decisions up front can make life easier down the road.
Adam: Dr. Rogers, I’ve got to ask you a big question I’m sure patients are wondering. What is your number one piece of advice for a patient who needs a mitral valve replacement?
Dr. Jason Rogers: My advice to patients is to ask questions, think about what’s important to you, make sure you have time to understand. It’s your body, and you should understand what’s being done. Never fear seeking a second opinion if what you’re hearing isn’t quite what you expected.
Adam: Dr. Rogers, fantastic advice. Thanks for sharing that with our patients. As always, thank you for taking time away from your very busy practice there at UC Davis in Sacramento and sharing these wonderful insights and innovations with our community.
Dr. Jason Rogers: Thank you, Adam. It’s always a pleasure to talk to you and with your audience. The most important thing to us is our patients and their outcomes. We really enjoy sharing this information with you and your audience at HeartValveSurgery.com. Thank you again.





