Ross Procedure Reloaded: What Should Patients Know?
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Chris Burke, MD, Co-Director, Multi-Disciplinary Thoracic Aorta Program, UW Medicine Heart Institute
Page last updated: January 17, 2024
There is no doubt about it.
Patient interest specific to the Ross Procedure continues to rise. My inbox continues to receive question-after-question from patients curious about this advanced form of aortic valve surgery that replaces a patient’s diseased aortic valve with the patient’s own pulmonary valve.
For example, Alexander, a patient with aortic stenosis and aortic regurgitation just emailed me, “Hello Adam – After extensive research, I’ve settled on the Ross Procedure as the best option since I have an active lifestyle and do not want to be on blood thinners. How can I find out the surgical outcomes and volume for Ross Procedure surgeons?”
I was fascinated to learn that UW Medicine Heart Institute in Seattle, Washington has launched a unique Ross Procedure Program that is led by Dr. Chris Burke, an aortic valve and root specialist. To better understand this “Ross Procedure Resurgence”, I was lucky to interview Dr. Burke.
Key Learnings About the Ross Procedure
Here are several key points that Dr. Burke shared during our interview:
- Dr. Burke decided to become a cardiac surgeon after “falling in love” with the specialty during medical school given the ability to restore heart function, the challenging nature of the procedures, the team environment and the positive impact heart surgery can have on patient health.
 Dr. Chris Burke
Dr. Chris Burke
- Today, Dr. Burke’s surgical specialties include thoracic aorta disease, aortic aneurysms, and aortic valve disease including the Ross Procedure and aortic valve repairs.
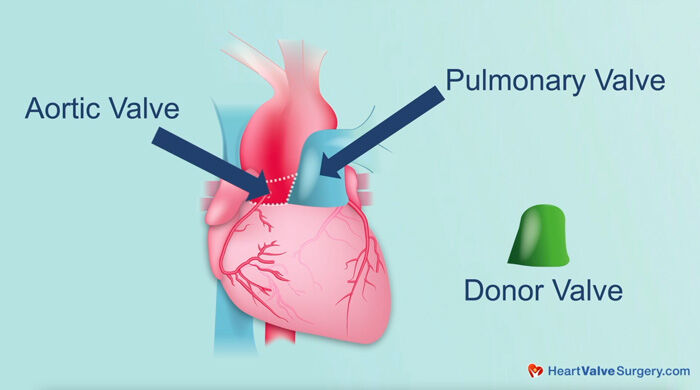
- The Ross Procedure is a “two-valve” procedure in which the patient’s diseased aortic valve is replaced with the patient’s pulmonary valve (the autograft). Then, a human donor valve is implanted in the pulmonary position (the homograft). For this reason, the Ross Procedure is sometimes referred to as the “Switch Procedure”.
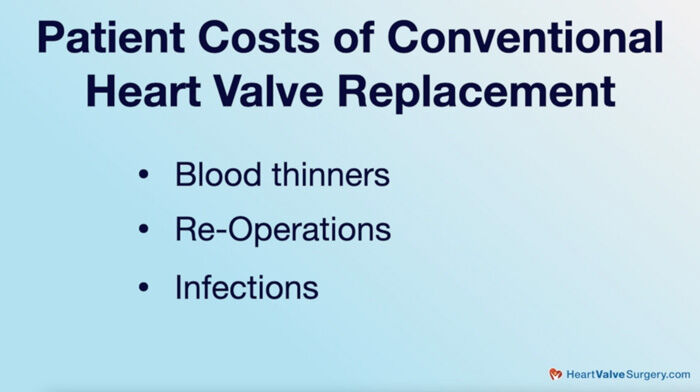
- Throughout his career, Dr. Burke observed several “patient costs”, or disadvantages, specific to conventional aortic valve replacements including the use of blood thinners, re-operations and infections. For these reasons, Dr. Burke evaluated the Ross Procedure as a unique approach to better suit the needs of his patients. As Dr. Burke states, “I really thought to myself, there has to be a better way we can do this. We must have some sort of innovation that can improve on these challenges. That coincided with data coming out showing the Ross Procedure in adults was both very durable and very safe.”
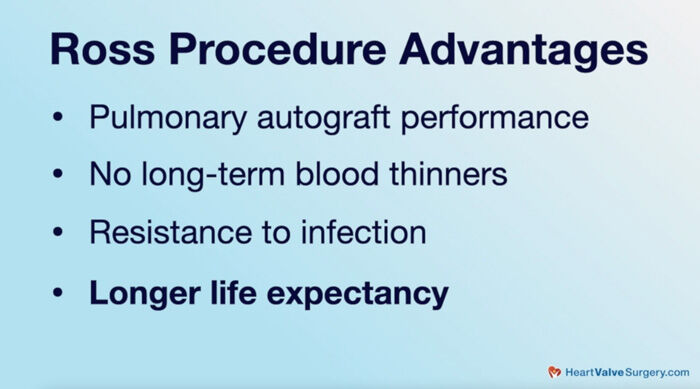
- According to Dr. Burke, there are multiple advantages of the Ross Procedure including (i) the performance of the pulmonary autograft, (ii) there is no need for patients to be on blood-thinners, (iii) the Ross Procedure is resistant to infection, and (iv) longer life expectancy. Dr. Burke states, “Most importantly, patients with the Ross Procedure tend to live the longest, and there’s some suggestion they may live as long, or close to, their age-matched peers who don’t have aortic valvular disease.”
- The Ross Procedure is sometimes dismissed by physicians. According to Dr. Burke, the Ross Procedure is a difficult procedure that requires a unique skill set to complete. Dr. Burke states, “It’s a hard operation. Conventional aortic valve replacement, certainly by cardiac surgical standards, is a fairly straightforward operation… A Ross procedure is a significant step-up from a technical complexity standpoint. It requires a full root replacement in most circumstances and a safe harvest of the pulmonary autograft, which has potential pitfalls. The pulmonary valve needs to be reconstructed. So, it’s many more operative steps. That gets into the critical importance for patients to be at a cardiac center that has experience with the Ross Procedure.”

- The Ross Procedure Program at the UW Medicine Heart Institute launched in 2019 with a dedicated, multi-disciplinary team to support patients. Dr. Burke states, “I had the commitment from my colleagues both on the surgical side, on the cardiology side, and on the entire treatment team. It’s important to realize this is not just simply a surgeon performing the procedure. There’s a whole team and program aspect. We weren’t going to do this if we were only 50% in. We had to be fully committed.”
- Many protocols were established by UW Medicine Heart Institute specific to the performance of the Ross Procedure and the personnel needed to maximize results (safety, effectiveness and durability).
 UW Medicine (Seattle, Washington)
UW Medicine (Seattle, Washington)
- The Ross Procedure Program at UW Medicine Heart Institute has grown quickly. This year, Dr. Burke plans to perform between 30 to 40 Ross Procedures.
- Patient age can be a factor when evaluating the Ross Procedure as a treatment option. Dr. Burke states, “In my practice… For patients with non-repairable aortic valve pathology, who are under 60 years old, a Ross Procedure is very much a first or frontline therapy. For patients aged 60 to 65 , it becomes a case-by-case consideration. I use age more as a surrogate for expected life expectancy. I want to see about 25 years or so. Much less than that if a patient has many co-morbidities or is over 65.”
- Dr. Burke believes the trend to the Ross Procedure will continue. According to Dr. Burke, “Patients are very savvy now. Patients do their research. I think that has been combined with the phenomenon that we’re seeing and appreciating that conventional valve replacement is maybe not such a great option in certain younger patient populations along with really good data showing the Ross Procedure to be a very safe, very effective procedure.
- The number one piece of advice that Dr. Burke has for patients is to do your research. “This is a technically demanding procedure,” states Dr. Burke. “The surgeon and programmatic volume does count and does have an impact. Seek high-volume programs. Make sure you are comfortable with your surgeon, and as a patient, make sure you’re comfortable with the environment that you’re in because ultimately that has a huge influence on outcomes.”
Many Thanks to Dr. Burke & UW Medicine Heart Institute!!!
On behalf of our entire patient community, many thanks to Dr. Burke for sharing his clinical experience and research with our community! Also, many thanks to the UW Medicine Heart Institute for taking such great care of heart valve patients!
Related links:
- See Dr. Burke’s Interactive Surgeon Profile
- Explore the UW Medicine Heart Institute Valve Microsite
- Ross Procedure: 10+ Facts to Know
Keep on tickin!
Adam
P.S. For the hearing impaired members of our community, I have provided a written transcript of my video interview with Dr. Burke below.
Video Transcript:
Adam Pick: Hi, everybody, it’s Adam with heartvalvesurgery.com, and this is a special surgeon question and answer session all about the Ross procedure. I’m thrilled to be joined by Dr. Chris Burke, who is a leading cardiac surgeon at UW Medicine Heart Institute in Seattle, Washington. During his fantastic career, Dr. Burke has performed over 1500 cardiac procedures in which more than 1,000 involved some form of valve repair or valve replacement. Dr. Burke, it is wonderful to have you here today with us.
Dr. Burke: Thank you, Adam. It is great to be here.
Adam Pick: Yeah, so we’re going to be talking all about the Ross procedure, but first I have a question about you. Why did you want to become a cardiac surgeon?
Dr. Burke: In many ways, I stumbled into the field a little bit, so I was in medical school, and I did a rotation on the thoracic surgical service, actually, doing lung and esophageal surgery and very much fell in love with the anatomy and the procedures, met some fabulous mentors, and from there, did a rotation in cardiac surgery and almost immediately fell in love with the specialty, the amazing impact on patients’ lives and the ability to restore function in the heart, the challenging nature of the procedures, the functioning in a team environment. All of those things came together. I knew it was a perfect fit, and I was very much motivated to dedicate my life’s work to this.
Adam Pick: Dr. Burke, there are a lot of things that you could focus on in cardiac surgery, but you chose a path all about valves. Why is that?
Dr. Burke: Adam, that related a bit to when I was in training here at the University of Washington and was in discussions to stay on as faculty. I saw that there was an opportunity here to help build the thoracic aortic program and aortic valve program, and that very much aligned with my clinical interests. I was very fortunate enough to be able to train after my residency training out at the University of Pennsylvania with Joe Bavaria and did his thoracic aortic super fellowship out there. Came back and from there things have really taken off. I treat all aspects of thoracic, aortic disease, aneurysms, dissections, and aortic valvular disease including aortic valvular repairs and Ross procedures, and it’s become my clinical and research passion and is pretty much almost exclusively what I do clinically now.
Adam Pick: Dr. Burke, you just mentioned the Ross procedure has become one of your specialties. I’m curious what attracted you to that two-valve procedure.
Dr. Burke: It really started when I was just observing what was happening with my patients and other patients around me. I really started to appreciate the cost that patients would incur following a conventional valve replacement, especially young patients, be it blood thinners, reoperations, infections, what have you. Especially in the era of TAVR, where more and more and more younger patients have been getting prosthetic valves, I’ve just seen patient after patient who’s only a few years out from their original surgery sitting in a cardiac surgeon’s office again in dismay over the prospect of having another surgery. I really thought to myself there has to be a better way that we can do this, and we must have some sort of innovation that can improve on this. That coincided with actually quite a bit of data coming out showing the Ross procedure in adults was both very durable and very safe, and so it was really a combination of those two things that led to me saying this is something we need to offer at the University of Washington.
Adam Pick: Dr. Burke, I love how you contextualize the cost for patients who have a need for a reoperation for an aortic valve replacement and I love how you touched on the Ross procedure as a potential long-term fix for that patient. I’m sure there are people watching this video who have never heard of a Ross procedure before. Can you explain for patients what it is?
Dr. Burke: The Ross procedure involves moving the patient’s own pulmonary valve over into the aortic position. After we do that, we actually reconstruct the pulmonary valve with typically a cadaver or a human pulmonary valve, so the patient’s left with two biologic valves both on the left side or aortic side, which we sometimes call the autograft or the pulmonary autograft, and then on the right side, which the pulmonary homograft.
Adam Pick: Dr. Burke, can you share with the patients what are the advantages of this two-valve procedure?
Dr. Burke: There’s multiple advantages, Adam. Pulmonary autograft serves as an excellent substrate for a neoaortic valve. There’s no need for blood thinners long-term. The Ross procedure is very resistant to infection. Most importantly, patients with the Ross procedure tend to live the longest, and there’s some suggestion they maybe live as long or close to their age-matched peers who don’t have aortic valvular disease. I think in young patients, that is of crucial importance.
Adam Pick: Dr. Burke, you may know this, but given all those advantages, I went ahead, and I selected a Ross procedure for myself all the way back in 2005, so I’ve realized those benefits, but at the same time, I understand that the Ross procedure may be also dismissed by some physicians out there. Can you talk about that?
Dr. Burke: It’s a hard operation. Adam, conventional aortic valve replacement certainly by cardiac surgical standards is a fairly straightforward operation, and it’s within the armamentarium of really any practicing cardiac surgeon. A Ross procedure is a significant step up from a technical complexity standpoint. It requires a full root replacement in most circumstances and prior to that a safe harvest of the pulmonary autograft, which has potential pitfalls. The pulmonary valve needs to be reconstructed, so it’s many, many more operative steps. It’s a longer procedure. There is more opportunity for things to go wrong, and that gets into the critical importance of being at a center that has experience with the Ross, is dedicated and committed to it, and does them in a high volume.
Adam Pick: Dr. Burke, you just mentioned the importance of experience and safety for patients having a Ross procedure. I understand that at UW Medicine Heart Institute, you have been a key figure in the launch of a Ross procedure program. Is that correct, and if so, can you share with our patients what has happened with the launch and the growth of that program?
Dr. Burke: We launched an adult Ross program here at the University of Washington about two years ago now. I partnered up with one of our surgeons at Seattle Children’s who had had some experience, and we were very selective early on, and I made sure that we had an institutional commitment to it, that I had commitment from my colleagues both on the surgical side, on the cardiology side, and on the entire treatment team. It’s important to realize this is not just simply a surgeon performing the procedure. There’s a whole team and program aspect that has to go in, and we weren’t going to do it if we were 50% in. We had to be fully committed.
We came up with a protocol for how we would execute the operations and what the personnel would be needed for these operations to maximize results because I knew that a microscope would be on us and I knew the importance of volume and experience, and we set all the pieces in play, and now we’ve – we’re building a program where this year we’ll do between 20 or 30 Ross procedures in this calendar year, so we’re very excited about that.
Adam Pick: Dr. Burke, on behalf of all the patients out there who are benefiting from your commitment and the commitment of your team there at UW Heart Institute for the Ross procedure, I can’t thank you enough. It’s interesting because I’ve noticed I would say within the last three years or so the number of emails I get in my inbox from patients, from parents about the Ross procedure has skyrocketed, and I’m just curious to know. Is there a new appreciation for the Ross procedure?
Dr. Burke: Absolutely, Adam. We’ve seen a similar trend here. I think there’s a variety of reasons for that. Patients are very savvy now, and there’s many, many resources available. Patients do their research. Heartvalvesurgery.com is certainly included in that category, and word travels and word gets out, and I think that has been combined with the phenomenon that we’re seeing and appreciating that conventional valve replacement is maybe not such a great option in certain younger patient populations along with really good data from many, many different centers from around the world showing this to be a very safe, very effective procedure. I think it’s both on the surgeon and cardiology aspect along with on the patient side of things and doing their own due diligence and research and seeking out high-volume programs.
Adam Pick: Dr. Burke, I heard you reference that the Ross procedure might be suited for younger people, but I’m curious to know is there some form of upper age limit where the Ross procedure might not be applicable?
Dr. Burke: Yeah, that’s a great question, Adam. In my practice, patients with non-repairable aortic valve pathology who are really under 60 years old, a Ross is very much a first or frontline therapy, so I would say anybody under 60 who has – who is otherwise in reasonable health. For me personally, 60 to 65 comes into a case-by-case basis. I use age more as a surrogate for expected life expectancy, and I want to see about 25 years or so. Much less than that if a patient has many comorbidities or is over 65. You’re probably not deriving the full benefit of the Ross procedure, and I think at that point, we would think a little bit more seriously about a bioprosthetic valve or even a TAVR in certain circumstances in those patients.
Adam Pick: Dr. Burke, while I have you here, I have to ask you the big question that I’m sure a lot of patients are wondering, which is what is your number one piece of advice for a patient or a parent who might be considering the Ross procedure?
Dr. Burke: Do your research. We wouldn’t buy a car without going online, doing research, talking to people who had bought similar cars or whatever, and I think the same thing is true here. We know the importance – especially for something like a Ross procedure. This is a technically demanding procedure, and the surgeon and programmatic volume does count and does have an impact. I think seek high-volume programs. Make sure you are comfortable with your surgeon, and as a patient, make sure you’re comfortable with the environment that you’re in because ultimately I think that has a huge influence on outcomes as well.
Adam Pick: Dr. Burke, fantastic advice, and on that note, I want to extend a huge thank you for taking time away from your very busy practice there at UW Medicine Heart Institute in Seattle, Washington to educate our patients about the Ross procedure.
Dr. Burke: Thank you, Adam. Thank you for all you do for our patients and the community, and it’s been fun.