Dressler’s Syndrome: What Does Steve Want All Patients To Know?
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Published: December 17, 2024
As we have seen many times in our community, patients going through heart valve surgery often turn a metaphorical lemon into lemonade. We “pay it forward” as they say.
For this reason, I wanted to share the story of Steve Deller. Yes, Steve is a heart valve surgery patient. Yes, Steve experienced complications after surgery. And yes, Steve wants to help future patients learn about Dressler’s syndrome.

Steve’s Shocking Diagnosis
In a wonderful email to me, Steve shared this:
My aortic valve replacements journey started back in June 2013 at the age of 55. My primary care physician (PCP) asked if I ever had my heart murmur “evaluated” before. I said, “No”. I have always had it and was told it was a “functional” murmur when I was younger. Whatever that means. My PCP referred me to have my first ultrasound of my heart to be done and evaluated.
I was diagnosed with a congenital bicuspid aortic valve with stenosis and severe insufficiency. I was counseled by my cardiologist at that time to have “preventive valve replacement” to prevent me from experiencing symptoms before they occurred. I was shocked about the diagnosis and extremely fearful of having open heart surgery. This seemed like a nightmare. After much more discussion, education, lots of prayer, love, and encouragement from family and friends, and the wonderful support of my wife, I decided to have my valve replaced at the Meijer Heart Center in Grand Rapids, Michigan, based on the recommendation of my cardiologist who knew of a highly skilled surgeon who has done a lot of this specific type of procedure.
Pig Valve & TAVR Failures
I was able to have it replaced with a pig valve through a minimal-invasive 3-inch lateral chest incision between two ribs and not have my sternum cut. They did have to cut off a piece of one rib that was in the way. I was thankful to hear that they didn’t have to cut down the length of my sternum with this first surgery.
Unfortunately, this first valve only lasted 10 years. The echo was showing “severe stenosis” again already. I was very disappointed to say the least. Upon more counseling with my cardiologist, I was eligible to have a TAVR procedure done which I had done in May 2023. However, after the TAVR was deployed, it totally compromised the blood flow of my main coronary artery. So, they went ahead and put a stent in the artery.
Six months later… I started having moderate-to-severe angina with exertion. I didn’t realize what was going on since I never had chest pain before. After two weeks of it not going away and seemingly getting more frequent, I finally reported these symptoms to my cardiologist. He referred me to immediately have a cardiac catheterization done. It showed 95% blockage of the stent, and my newer valve did not seem to be working properly. I was devastated, and quite fearful of maybe losing my life.

A Mechanical Valve & Bypass Surgery
I was immediately admitted to the cardiac unit for observation for 5 days. They could not perform open heart surgery on me until my Plavix medication tapered off due to its long half-life to prevent excessive bleeding during surgery. It was explained to me that the only way to fix the stent blockage was to perform open heart surgery and do a double-bypass around the blockage and remove the other two pig valves. My surgical team and myself decided it would be best to put in a larger 27mm mechanical valve for hopefully life-long management.
The first valve that was done in 2013 was technically a valve that was too small for my body size and a “patient prosthesis mismatch”. I also was never educated on the fact that stents “can fail” and get plugged up, and cause angina. That is why I waited so long to report my symptoms as I wasn’t sure what was going on, especially with just having a “new” valve put it. I almost waited too long.
Post-Op Pleural Effusions
Again, I had to put my life in the hands of my cardiology professionals and trust God to help me survive this very invasive surgery. Praise the Lord, the nine-hour open heart surgery was successful. However, I ended up having the post-surgery complication of recurrent pleural effusions. I had two thoracentesis procedures done while I was still recuperating in the hospital.
This is where things went wrong for me and got rough. Every two weeks over the next two months, my pleural space continued to fill up with over 1200 mLs of fluid.
This was scary to me and made it hard to breathe. After the third and fourth times this occurred, I kept asking my surgeon and cardiologist, “Why does this keep occurring to me, and what could be causing this?”
I was told, “We are not totally sure. We will just have to wait-and-see if it will stop on its own. If it doesn’t, we can refer you to have a pleurodesis procedure done.”
After researching what was done during that procedure, I decided I did not want that lung tissue destruction done to me. This option was not acceptable to me. I needed this complication to stop sooner than later. So, I became my own best self-advocate, and researched a prominent pulmonologist downstate, hoping he could help figure out what was causing my recurring pleural effusions.
Possible Dressler’s Syndrome?
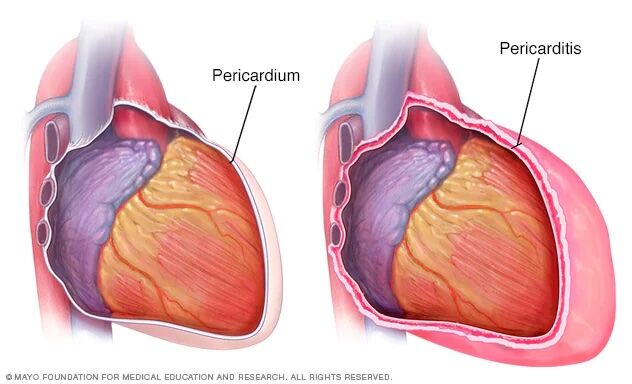
After seeing me, the pulmonologist diagnosed that I may be experiencing a condition called Dressler’s Syndrome, an autoimmune inflammatory reaction my body was responding with to the heart tissue surgery that was done. He recommended I start taking Motrin 1000 mg daily and colchicine 0.6mg daily for the first several weeks, and then he titrated me down over the next five weeks.
Finally, after having my sixth thoracentesis done, my pleural space filling finally stopped!
This treatment worked for me….. Finally!
I was so relieved.
Steve’s Dressler’s Syndrome Takeaways
I share my experience and story with you, because here are my important learning takeaways from this last surgery that I would like to share with everyone. I have learned that if you have more than two pleural effusions after open heart surgery like I did, you should consult with your surgeon about having blood work done for inflammatory markers for possible Dressler’s Syndrome. They doctors nothing about this condition, therefore, could not offer me treatment for this complication which is quite simple. It may have saved my going through four unnecessary expensive thoracenteses procedures if this condition was caught much earlier.
I have learned this condition is rare to occur and is usually seen after myocardial infarction patients, but it can still occur with open heart surgery patients too! I read about this condition and the pleurodesis procedure first on the MayoClinic.com website. I also learned that having a stent placed in your artery “can fail.”
They can get plugged up and stenosed on their own, and you should be taught to report any chest pain/angina after having a stent placement. I was clueless to this phenomenon.

Thankful and Getting Back To Life!
I am just so very thankful to still be alive and doing better.
I still get short of breath on exertion, but I do walk daily and started playing pickleball a couple times per week to keep moving. My cardiologist has recommended that I keep taking the colchicine for up to a year. I will be titrating the dose down over the next two months to see if I can “wean” off of it.
I understand that Dressler’s Syndrome can flare up again. Please pray that mine doesn’t, and I can permanently be taken off of long-term colchicine therapy. So, there you have it. Hope this story helps someone else not go through six thoracenteses procedures like I had done. Thank you everyone for all of your prayers, love, and support during the past 10 months.
I appreciate it more than you will ever know.
Keep on tickin!
Steve