Janet’s Patient Success Story: Why I Got A Mitral Valve Repair Surgery
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Dr. Marc Gerdisch, Chief of Cardiac Surgery at Franciscan Health
Published: January 17, 2023
Patients diagnosed with mitral regurgitation are often confused about the long-term advantages of a mitral valve repair compared to a mitral valve replacement. Additional patient confusion may come from the fact that mitral valve repair is not performed by all surgeons given this advanced surgical technique.
Janet Peterson, however, was not a confused patient. Janet knew she wanted a mitral valve repair. And, Janet knew the surgeon she wanted to perform her surgery. This is Janet’s patient success story.
Key Learnings From Janet’s Story
Important learnings shared by Janet and Dr. Gerdisch in this interview include:
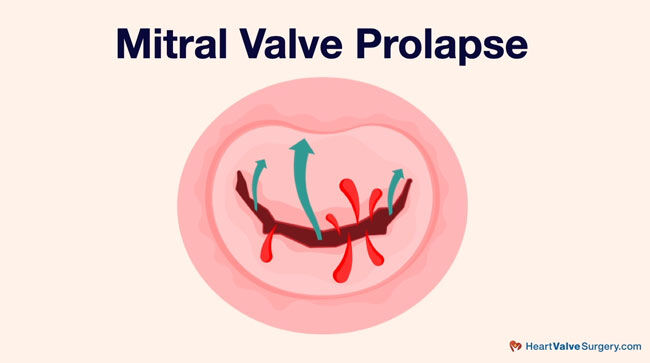
- Janet, a retired accountant, was diagnosed with mitral regurgitation after she fainted at work 20 years ago due to mitral regurgitation, a leaking heart valve.
- Following her initial diagnosis, Janet learned about the advantages of mitral valve repair from her cardiologist who previously had a mitral valve repair surgery. “I remember when I was diagnosed with the mitral valve prolapse back in the early 2000s, my general physician also had mitral valve prolapse,” states Janet. “I remember him saying it’s important that you catch it and have it repaired not replaced.”
- For 20 years, Janet was in ‘watchful waiting’ until 2022 when the mitral regurgitation became severe. Although Janet was asymptomatic (without symptoms), she needed surgery.
- Specific to mitral regurgitation symptoms, Janet may not have experienced shortness of breath, fatigue or chest pain, but Dr. Gerdisch has a different interpretation of what symptoms can be. Dr. Gerdisch states, “For me, any additional changes on the echocardiogram, in my mind, are symptoms. That’s a picture of your heart. If I see anything change about the movement of the heart, the strain of the ventricle, dimensions of atria, the other valves perhaps showing some signs… for me those are symptoms.”
 Mitral Valve Opening During Transesophageal Echocardiogram
Mitral Valve Opening During Transesophageal Echocardiogram
- When Janet researched the local cardiac surgeons near her hometown of Wadesville, Indiana, she did not find any surgeons who repaired mitral valves. The surgeons near Janet’s hometown only performed mitral valve replacement. Janet states, “It was really important for me to find a surgeon whose focus was on repairing and not replacing because replacing the valve was the only thing my local cardiologist had recommended. My research showed that I would need to go outside the metro area where I live in order to find a good surgeon to do that.”
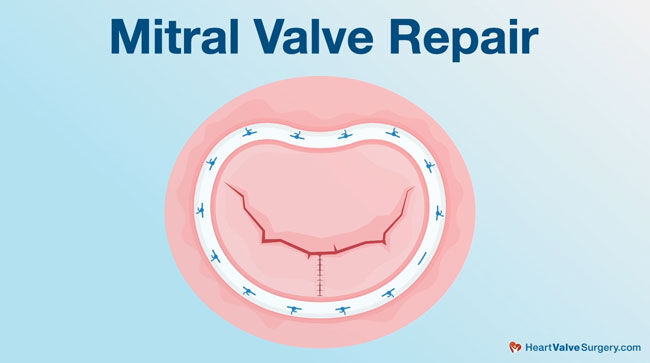
- According to Dr. Gerdisch, when a mitral valve repair is performed by an experienced surgeon at a hospital that specializes in mitral valve repair, the patient can return to a normal life expectancy. “Janet’s survival is no different than a neighbor who doesn’t have these valve issues,” states Dr. Gerdisch. “When we have to replace a valve, although replacement valves are marvelous devices, they’re brilliant, they do save lives, they extend lives, they don’t give us the opportunity to restore the entirety, potentially, of a person’s entire life because the prosthetic valve carries risk with it.”
- Janet researched surgeons at HeartValveSurgery.com. Janet states, “When I Googled “mitral valve repair, Indianapolis, Indiana,” your website came up. The very first video I found was the one that talks about minimally invasive surgery.”
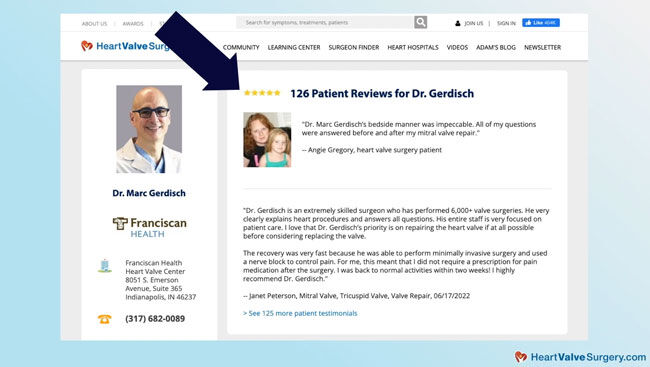 Janet’s Online Research Helped Her Find Dr. Marc Gerdisch
Janet’s Online Research Helped Her Find Dr. Marc Gerdisch
- After much consideration and discussion with Janet about her options, Dr. Gerdisch performed a minimally-invasive mitral valve and tricuspid valve repair on Janet. While Dr. Gerdisch performs many heart valve surgeries via minimally-invasive approaches, safety is the key consideration for Dr. Gerdisch as he tailors the surgical approach for each specific patient.
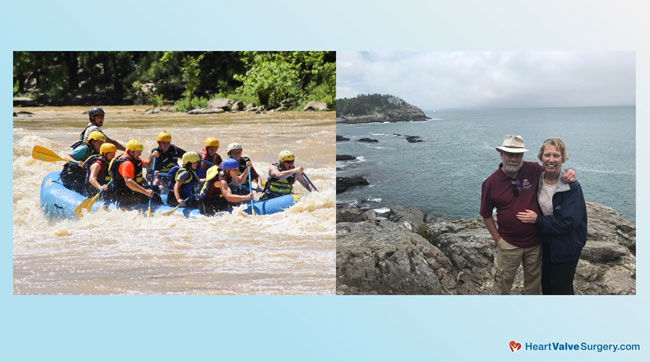 Janet After Heart Surgery – Rafting with Family & Traveling
Janet After Heart Surgery – Rafting with Family & Traveling
- Janet’s recovery from heart surgery was quick and Janet did not need prescription pain killers (e.g. opioids). “When I left the hospital, I don’t think I was on anything. I think I took Tylenol a few times and that was really all I needed. I didn’t need the nerve medication or any of that. I forget what the name of the cryo technique that Dr. Gerdisch uses but that definitely worked.”
- When reflecting on her surgery, Janet considers the operation a “speed bump on the highway of life”. Janet states, “My advice to patients would be research as much as you can. You have to be comfortable with the surgeon that you choose. Research it as much as you can, meet with them, meet with multiple surgeons if you need to and make the decision that’s right for you.”
Many Thanks to Janet, Dr. Gerdisch & Franciscan Health!
On behalf of our entire patient community, many thanks to Janet for sharing her story and Dr. Gerdisch for sharing his clinical experience and research with our community! Also, many thanks to the Franciscan Health team for taking such great care of heart valve patients.
Related links:
- Surgeon Insights: Minimally-Invasive Mitral Valve Repair
- Surgeon Q&A: Will I Need Mitral Valve Surgery?
- Atrial Fibrillation: A Concern for Mitral Valve Patients
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our community, I have provided a written transcript of my interview with Janet and Dr. Gerdisch below.
Video Transcript:
Adam Pick: Hi, everybody! It’s Adam with heartvalvesurgery.com and this is a special mitral valve repair patient success story.
I am thrilled to be joined by Dr. Marc Gerdisch, who’s the chief of cardiac surgery at Franciscan Health in Indianapolis, Indiana. We are also joined by Janet Peterson, his patient who’s a retired accountant from Wadesville, Indiana.
Dr. Gerdisch, it is great to see you again and thanks for being with us today.
Dr. Gerdisch: My pleasure, Adam. Glad to be here, thanks.
Adam Pick: Janet, I am really excited to hear about your journey through heart valve surgery and thank you for being with us today.
Janet Peterson: You’re welcome. I am happy to be here.
Adam Pick: Janet, to get started, let’s hear a little bit about your story. What were you diagnosed with, when were you diagnosed and what happened next?
Janet Peterson: I was diagnosed with mitral valve prolapse and that happened in, probably, the early 2000s. As we talked a little bit earlier, I lived in Southern California and was working there, and I happened to faint one day at work. They hauled me off to the ER and they were actually looking for a rhythm problem or something to explain why I fainted. They did every kind of test they could come up with and mitral valve prolapse was what they eventually diagnosed me with. For the last 20 years, we’ve just been monitoring that, and it all came to a head this year.
Adam Pick: Janet, when you say it came to a head, what specifically do you mean?
Janet Peterson: Well, my cardiologist and I were doing annual echocardiograms, just to monitor how the mitral valve prolapse was doing and there were no issues. I know a lot of people— I’ve read all the information on your website and online about how a lot of people will make it and never have to have heart valve surgery with mitral valve prolapse, but the leaflets of my mitral valve got to the point where the echocardiogram in 2022 showed that there was serious regurgitation. My cardiologist mentioned the word “surgery” for the first time and that’s when I delved into online research and trying to figure out who would be best to fix it for me.
Adam Pick: Janet, you’re diagnosed, you go through a very long period of watchful waiting, then you hear, it’s time for surgery. You do some research and then what happened?
Janet Peterson: Well, I had no symptoms and the last meeting I had with my cardiologist after he told me the results of the echocardiogram, he kept asking, “Do you have symptoms?” and my response was no. I had to make a decision and do the research on my own and your website was a huge help with this, as to whether I wanted to go ahead with surgery or wait for symptoms. I remember when I was diagnosed with the mitral valve prolapse back in the early 2000s, my general physician also had mitral valve prolapse. I remember him saying it’s important that you catch it and have it repaired not replaced.
My local cardiologist in the local heart group here in southern Indiana, the research that I did, I did not see that they did any repairs, it was replacing the mitral valve. That was my main focus, finding someone who I was comfortable with that could repair it. One of the videos on your website talks about the importance of repairing and not replacing, so that was where my focus was.
Adam Pick: Dr. Gerdisch, let’s unpack some of Janet’s story here. Mitral regurgitation with no symptoms. Is that common and can that be a problem for both the patient and the physician cardiologist who’s watching that patient?
Dr. Gerdisch: Really interesting points and Janet tells her story perfectly so there’s very little for me to add, other than to embellish on a couple of the points that she already made. First of all, she just had mitral valve prolapse without much regurgitation and only about 5% of those people go on to have severe mitral regurgitation and then she had more regurgitation. When you get to the moderate range, about half of those people will go on to have severe mitral regurgitation, so she just took us on the organic journey of what happens with the valve.
Then with respect to symptoms, in my mind it’s always what are we going to classify as symptoms. Yes, of course, symptoms that you experience in your daily activities, you become short of breath, you have palpitations that kind of thing, also for me, any additional changes on the echocardiogram. In my mind, those are symptoms. That’s a picture of your heart. If I see anything change about the movement of the heart, the strain of the ventricle, dimensions of atria, the other valves perhaps showing some signs, for example, leaking in the tricuspid valve that we need to address, for me those are symptoms. Janet is unlikely to complain about something because she has reserves, she has physiological reserve. She’s the perfect story of somebody that you really need to stay on top of.
Adam Pick: Janet, mitral valve repair was obviously very important. You did a lot of research to find someone who specializes in that technique. Why, if you can remember, was it so important for you to get a mitral valve repair?
Janet Peterson: My general physician, when I was first diagnosed in the early 2000s, had the same condition, so he shared with me the importance of catching it. That was actually my biggest fear when I went to see Dr. Gerdisch and have the consult with him that even though I wasn’t having symptoms that I might have waited too long and wouldn’t be able to get it repaired. It was really important for me to find a surgeon whose focus was on repairing and not replacing because replacing the valve was the only thing my local cardiologist had recommended. My research showed that I would need to go outside the metro area where I live in order to find a good surgeon to do that.
Adam Pick: Dr. Gerdisch, mitral valve repair, very big topic in our community. Can you maybe share, for the folks out there who are newly diagnosed, what are some of the really big benefits of a mitral valve repair compared to a replacement.
Dr. Gerdisch: I’m going to front-end load it a little bit because we just talked about the importance of meeting that challenge early. In other words, when you identify severe mitral regurgitation that it be addressed at that stage, before there are permanent changes in the heart. The reason that’s important is because we know that when we intervene with severe mitral regurgitation, before there are structural changes in the heart, then we can restore a person’s normal live curve. Somebody like Janet, for whom we intervened at a very good time, with her heart muscle still normal– as I recall, Janet, we also fixed your tricuspid valve, didn’t we?
Janet Peterson: We did, yes.
Dr. Gerdisch: Yeah, so timing was ideal. We treated that as well, which can be a chronic and enduring problem that we can even cover later; it’ll never be a problem for her. Doing so, we were able to put people– really, Janet’s survival is no different than a neighbor who doesn’t have these valve issues. When we have to replace a valve, although replacement valves are marvelous devices, they’re brilliant, they do save lives, they extend lives, they don’t give us the opportunity to restore the entirety, potentially, of a person’s entire life because the prosthetic valve carries risk with it. Adam, you’ve heard me say before, trading diseases. When we replace a valve, we trade diseases. We go from this really threatening disease to a much less threatening but still a disorder.
A mitral valve repair, if we have somebody who has repairable anatomy and we can’t repair it, it’s a pretty big defeat, quite honestly. It’s something I always prepare everybody for, for that very, very small possibility that we won’t be able to repair the valve. Those of us who do it a lot, we won’t give an inch on that. We are going to fix the valve any opportunity we have because of that difference, that distinguishing characteristic over the longevity of the patient, the entirety of their lives.
Adam Pick: Thanks for the explanation, Dr. Gerdisch. Mitral valve repair is big on your radar, Janet. How did you go about finding Dr. Gerdisch?
Janet Peterson: First thing I tried to do was find out if the local heart surgeons would be able to do that and I could not find anything online about local surgeons. Indianapolis, Nashville, some of the closer large metropolitan areas where I started to look and when I Googled “mitral valve repair, Indianapolis, Indiana,” your website came up. The very first video I found was the one that talks about minimally invasive surgery, which was not really on my list of things. I would have preferred the valve be repaired no matter what and I was okay with the sternotomy, not the minimally invasive but that was just icing on the cake, if you will, made the recovery a whole lot easier.
Adam Pick: Janet, it’s great to hear that the website helped you find Dr. Gerdisch. I’m curious to know, you make that call to his office, what was it like when you spoke to his team?
Janet Peterson: One of my sisters is a nurse and I took her along, just to get the feedback that she would have from that perspective. She and I kept saying, we knew it was not your first rodeo. We talked with the individuals there in the office, they’d got the medical background and then we talked to Dr. Gerdisch, and I was totally comfortable. It’s amazing to me I could make that big a decision in just having maybe a 20-minute conversation with him. I had my questions and I got confirmation on all the important points that I wanted to make sure of, which was repairing the valve, not replacing it if we could at all and all the other questions answered, and his team took it from there. I was there April 28th and surgery scheduled June 17th and a couple of weeks after that, I was back to normal.
Adam Pick: Dr. Gerdisch, Janet was set. She wanted a mitral valve repair, she couldn’t find it locally, she decided to come a couple of hours from her home up to you in Indianapolis. I’m just curious, do other patients struggle finding someone who specializes in mitral valve repair?
Dr. Gerdisch: There are centers that do this kind of work on a regular basis and particular physicians that do these types of operations on a regular basis and that’s where you want to be so that you do get a valve repair. I would echo Janet’s comment that the most important thing to her was having her valve repaired. Obviously, we love the minimally invasive approach, and we love to do that. In the vast majority of surgery, we do it through a small incision because it’s nicer for the patient and we can delivery exactly the same operation.
There are situations where that might not be so true. For example, I just presented a patient last weekend at a meeting we had in Boston that I had operated on just prior to that meeting because we needed a video for the meeting. It’s important for this context because that fellow was in his 70s, he had severe mitral regurgitation, atrial fibrillation and so far, he’s minimally invasive. We can fix those things minimally invasively, but he had calcium in the mitral valve. If there is any chance that the approach will affect my ability to repair the valve, then I do the approach that leads to the highest [likelihood 12:58 of] repair. In this case, for him it was a sternotomy so that I could decalcify the valve and still repair the valve. It’s a little bit more complex to do that through a small incision so we just don’t do it that way.
As Adam knows, in our practice everybody that we do a sternotomy for has a special process called [rate of sternal fixation 13:18], which it’s very hard for us to tell our minimally invasive patients from our sternotomy because of it. Everybody has an accelerated recovery, everybody has minimal discomfort, everybody gets back to work quickly, but we always want to tailor the situation for the patient. If the opportunity is there to be minimally invasive, then we do it. If that is our best approach that’s what we do. We change the approach based on the anatomy.
Adam Pick: Dr. Gerdisch, Janet was set on a mitral valve repair. She came up, saw you. I’m curious to know, what did you two come up with in terms of the treatment of her mitral valve.
Dr. Gerdisch: I think that’s a very important point that the two of us came up with a treatment plan. We discussed all the options. We tailored what her experience would be. We talked about her lifestyle, her expectations, how she sees her life in the future. You said, she was set on a mitral valve repair, so that was our first conversation, can we repair the valve, and I was certain we could repair the valve. We also saw that she had some leak in the tricuspid valve and that the anulus of the tricuspid valve was enlarged. When we see that, we should always take the opportunity to judge whether the patient will benefit in the long run from having that addressed.
In a case like Janet’s where it was leaking, where it was enlarged, she’s a young, healthy person, we should definitely address that valve. It’s important, of course, we do that in a fashion that doesn’t result in any untoward effects, but this is an operation we do over and over and over again, so we feel comfortable with it. For Jane, after we talked about that, after I brought that into the conversation as well, recognizing that both valves could be repaired, that was our initial goal was to get the valves fixed. Then looking at the operation from an anatomical standpoint, with respect to approach, with respect to safety, it was clear that Janet would be an excellent candidate for a minimally invasive double valve repair. That gave us the advantage of not only repairing the valves but lessening the tissue trauma, probably abbreviating the recovery a little bit and ensuring that the overall trauma to her and her life was diminished. Small incisions are nice in the sense that it also gives you a nice cosmetic result that then leaves you with less evidence of the operation.
Adam Pick: Janet, as you may have seen in some of these videos with Dr. Gerdisch, one of the things he’s known for is his rapid recovery protocol. I’ve got to ask you, what was your experience recovering from a mitral valve and tricuspid valve repair?
Janet Peterson: Much faster than I anticipated. I’m active anyway and I continued with my daily walks with my puppy and chicken coop cleaning and all of those things. I was back to doing all of that within a couple of weeks.
Adam Pick: Janet, one of the big concerns patients have is pain, in addition to that we’re in this opioid crisis. I’m curious, what was your experience with pain, and did you need pain medication during your recovery?
Janet Peterson: When I left the hospital, I don’t think I was on anything. They filled all the prescriptions for me at Franciscan Health and I took this big bag of pharmaceuticals home and I think I took Tylenol a few times and that was really all I needed. I didn’t need the nerve medication or any of that. I forget what the name of the cryo technique that Dr. Gerdisch uses but that definitely worked. I’ve had other surgeries where I was on pain medication, so I know what that feels like. I was amazed at the recovery because Tylenol was all I really needed.
Adam Pick: Janet, I’ve been lucky to get to know you here and I’ve heard you say that heart surgery is like a speed bump on the highway of life. What do you mean by that?
Janet Peterson: On my daily walks with my puppy, Sadie, I had a lot of things to think about, both before and after the surgery and I had no idea what to expect. You can prepare a person and you can do all the online research and find a great physician to do it, but you really don’t know what it’s like until you get through it. On the other side, I’m thinking, it really wasn’t so bad. It was, like you say, like a speed bump in the highway of life and it could have been a whole lot worse. I am just so thankful that I found Dr. Gerdisch and all of the individuals in his office at Franciscan Health, they were all great. It could not have gone better for me. I just retired so it was a good way to start retirement.
Adam Pick: Dr. Gerdisch, you see thousands of patients there at Franciscan Health in Indianapolis. I’m really curious, you just heard Janet tell her perspective of this wonderful experience under your care. How do you feel about Janet’s outcome?
Dr. Gerdisch: Janet is emblematic of the vast majority of patients who have an experience with us, which is wonderful. It’s just wonderful. It’s so thrilling every day to be surrounded by the team that we have that’s helping create this experience for the patients. I always say my job is the easy part because I get to do the work in the operating room. For me, it’s fun, enjoyable, intense, exciting, exhilarating and then I have all this wonderful staff that implement all of the things that lead to this type of recovery, that give people this very positive experience.
Adam Pick: Dr. Gerdisch, thanks for those insights about Janet’s recovery from your perspective. Janet, I’ve got to ask you, how are you feeling now?
Janet Peterson: I’m feeling fabulous. I have a long life to look forward to and I am just very thankful that I found Dr. Gerdisch and his team, and we got it taken care of. I don’t have to worry about it.
Adam Pick: You got it taken care of, for sure, thanks to Dr. Gerdisch and his team. Now, we’ve got to ask you the big question for all the patients out there who are watching this. What is your advice for patients who have just heard that they need heart valve surgery?
Janet Peterson: My advice would be research as much as you can. You have to be comfortable with the surgeon that you choose. Research it as much as you can, meet with them, meet with multiple surgeons if you need to and make the decision that’s right for you. I know for me it was 20 years of monitoring this situation and I know several of the videos that I watched say that it’s not necessarily an emergency, so you don’t need to make that decision today. It’s important to talk to as many surgeons as you need to, to find the one that you are most comfortable with.
Adam Pick: Janet, before we end this wonderful chat, this is a pretty special experience in which I get to see a patient with their surgeon talking about a successful operation. I’m curious, is there anything that you want to share with Dr. Gerdisch about his care and the care of his team?
Janet Peterson: I just want to say a big thank you to Dr. Gerdisch and his team. I know they all work in concert together, it made my experience just a speed bump in the highway of life, as we talked about. He’s so very humble is my take on it. The first day that I talked with him after the surgery and he explained to me what was done, I was just so thankful that we were able to repair it. His response to me, I believe and pretty much the same words were, he said it was my privilege. He said the valve tissue is in great shape and the heart muscle is strong and that to me was the best news ever, so I thank Dr. Gerdisch very much.
Adam Pick: On that wonderful note, we are going to wrap up the incredible story of Janet’s successful journey to a healthy heart. Janet, thank you so much for being with us today and sharing all about your experience with mitral valve and tricuspid valve repair surgery.
Janet Peterson: Thank you very much, Adam.
Adam Pick: Dr. Gerdisch, as always, thanks for taking time away from your very, very busy practice there in Indianapolis, Indiana at Franciscan Health.
Dr. Gerdisch: Thank you, Adam, it’s been a pleasure. Thank you, Janet, for taking the time to tell your story and share your experience about your time spent with us.