“Will I Need Mitral Valve Surgery?” asks Wolfgang
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Dr. Marc Gerdisch, Chief of Cardiac Surgery at Franciscan Health
Published: April 6, 2022
We just received a great question from Wolfgang about mitral regurgitation and the potential need for patients to undergo mitral valve surgery. In his email, Wolfgang writes to me, “Adam, I’m 25 years old. I’ve got mitral regurgitation between zero-to-one on a scale of four. I’m afraid that the disease will progress. Do most people with mitral regurgitation and mitral valve prolapse eventually need a repair or a replacement?”
To answer Wolfgang’s question, we contacted Dr. Marc Gerdisch, the Chief of Cardiac Surgery at Franciscan Health in Indianapolis, Indiana. During his 25+ year career, Dr. Gerdisch has performed over 6,000 cardiac procedures and more than 4,000 heart valve operations. At HeartValveSurgery.com, Dr. Gerdisch has successfully treated over 120 patients including Dan Rhoden just a few days ago.
Key Learnings About Mitral Valve Prolapse Surgery
Here are the key learnings that Dr. Gerdisch shared during our interview:
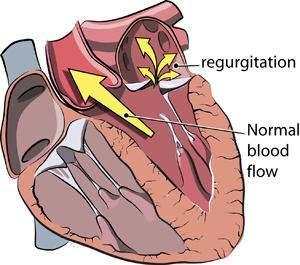
- Approximately 2% of the population have some form of mitral valve prolapse which causes blood to flow backwards, or leak, across the valve.
- Only a small subset of patients with mitral valve prolapse will need an operation.
- The likelihood that a patient will need surgery is determined by the severity of the leak. For patients with a mild leak, the worse-case scenario that a patient will need surgery in 5 years is 5%. For patients with moderate-to-severe mitral regurgitation, there is a 50% chance those patients will need surgery.
 Dr. Marc Gerdisch
Dr. Marc Gerdisch
- A key indicator for the progression of mitral regurgitation and the potential need for surgery is the size of the mitral annulus. Dr. Gerdisch states, “The only real predictor we have is the size of their annulus. If we look at folks who have moderate insufficiency, if their annulus, which is where the leaflets attach, or the size of the hole or the orifice, if it’s four centimeters or more, they have a considerably higher incidence of progression. Whereas folks who have smaller annuli, which makes sense, of course, because the leaflets are closer together, are less likely to progress.”
- To help patients manage and monitor their mitral valve disease, Dr. Gerdisch recommends seeing a cardiologist once a year. Over time, a cardiologist will be able to determine whether mitral regurgitation is progressing or not. If the “leakiness” of the valve is not progressing, the cardiologist may recommend that the patient be seen less frequently.

- Echocardiograms are excellent diagnostic tests for rating the amount of blood leakage across the valve. For patients with a 1 rating of mitral regurgitation, that is considered “normal”. For patients with a 1 to 2 rating, that is considered “mild”. When patients have a rating of 3 or more for their mitral regurgitation, that valve needs to be followed closer and is considered “moderate”. Any form of mitral regurgitation that is rated 4 or above will most likely need to be fixed and is considered “severe”.
- Dr. Gerdisch advises patients to be their own advocate and ask questions to their doctors about their heart and their heart valves. Dr. Gerdisch states, “I think people have to be their own advocates because doctors are looking at a lot of things, a lot of reports, and sometimes they don’t have time to really ferret through thee details. You shouldn’t be afraid to ask those questions.”
Many Thanks to Dr. Gerdisch & Franciscan Health!!
On behalf of our entire patient community, many thanks to Dr. Gerdisch for sharing his clinical experience and research with our community! Also, many thanks to the Franciscan Health team for taking such great care of heart valve patients.
Related links:
- Surgeon Insights: Minimally-Invasive Mitral Valve Repair Surgery
- Top 5 Facts About Dr. Gerdisch’s Rapid Recovery Protocol
- See 120 Patient Reviews for Dr. Gerdisch
Keep on tickin!
Adam
P.S. For the hearing impaired members of our community, I have provided a written transcript of the video with Dr. Gerdisch below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with heartvalvesurgery.com. Today, we’re answering your questions about the need for mitral valve surgery. I am thrilled to be joined by Dr. Marc Gerdisch who is the chief of cardiac surgery at Franciscan Health in Indianapolis, Indiana. During his extraordinary career, Dr. Gerdisch has performed over 6,000 cardiac procedures, of which more than 4,000 involved some form of heart valve repair or heart valve replacement. Dr. Gerdisch, let’s get started with this question from Wolfgang who asks, “Adam, I’m 25. I’ve got mitral regurgitation between zero to one on a scale of four, but I’m afraid that it can progress. Do most people with mitral regurgitation and mitral valve prolapse eventually need a repair or a replacement?”
Dr. Gerdisch: I’m really glad Wolfgang asked that question because I think it’s one to be answered to a wide audience. It’s one of the reasons that I love your site because people can – a lot of people can get this information out. Mitral valve prolapse is common. When we talk about mitral valve prolapse, we just mean that some portion of the valve comes up above the level of what we call the annulus, so it comes up out of the plane of where the leaflets attach. People have a leak with mitral valve prolapse. Of course, they’re concerned about that leak getting worse. Two percent of the people in the world have got mitral valve prolapse. That’s a lot of people, right? Only a small subset of them will progress to needing something done.
Let’s talk about Wolfgang. Wolfgang has a small leak, zero to one. If we look at the literature, the worst-case scenario for zero to one in five years is 5%. That’s a worst-case scenario of those patients will progress to severe mitral insufficiency. On the other hand, if you have mitral valve prolapse and you have moderate insufficiency, 50% of those people will progress in five years to severe insufficiency. The only real predictor we have of who those patients are is the size of their annulus. If we look at folks who have moderate insufficiency, if their annulus, which is where the leaflets attach, or the size of the hole or the orifice, if it’s four centimeters or more, they have a considerably higher incidence of progression, whereas folks who have smaller annuli, which makes sense, of course, because the leaflets are closer together, are less likely to progress. Now, that’s going to vary with the size of the patient, the size of their heart, whether they have other conditions, atrial fibrillation, etc., but those are the basic guidelines.
To answer Wolfgang specifically, very unlikely, Wolfgang, that you’re going to end up needing an operation. Wolfgang is going to say, “Well, you know what? I’m very in tune to my body. I want to be sure that I’m okay. How often should this be checked? Because Dr. Gerdisch just said five years. He didn’t say 10 or 15 years.” My answer to Wolfgang would be, number one, he should address his own level of anxiety. That’s important. Somebody wants to know if they feel like they hear a click or they’re getting palpitations or something, they should always get that checked out.
They should see their physician who knows how to evaluate their heart I think once a year. That only makes sense. You’ve got some condition, that should be checked. That person, that physician, will probably make the decision on how often to look. In Wolfgang’s situation, because if I had my first echo and I first saw that, I would want another echo in two years. It would look exactly the same. I’d push out to three years. If it looks exactly the same, I’d probably have a three-to-five-year schedule. I hope that makes sense, but these are serious issue for people. Initially, a little bit tighter window, and then as it’s completely stable and your heart’s normal, you can spread it out.
If you have moderate insufficiency, so three plus, not one plus or one and a half or two, if you have moderate leak in about two or three plus, those patients then need to be followed more closely, and that’s annually I think for those people to get a look at the valve and make sure that it’s stable.
Adam Pick: Wolfgang, I hope that helped you. I know it helped me. Dr. Gerdisch, I’ve got to ask you. Patients, we can be really confused. We see echocardiograms we don’t truly understand. We see results on diagnostic tests we don’t really understand. Real quick, can you talk maybe a little about the scale that Wolfgang was referring to, the zero, the ones, the twos, the threes, and how that relates to the severity of mitral regurgitation?
Dr. Gerdisch: That’s a great question. You’re right. People see their reports now. People have access to their charts and they read their reports. I’m going to take this in two directions. One is that a leak of a mitral valve of one plus is considered normal. Two plus is a little bit more than normal, but it doesn’t have any real consequence. Again, in two plus, if we follow those patients over time, there’s a low incidence of them progressing. When we get into three plus, that is a solid moderate leak and that needs to be followed closely. Four plus is severe and not only does it need to be followed closely, but most of the time, it needs to be fixed, even before there are any ill consequences to the patient, as long as they’re able to get to somebody who can with great certainty repair that valve. That’s the scale. Zero to one, that’s normal. One to two, including two, really mild and not something to be concerned about, but is worthy of some attention. Three, a lot of attention, four, usually needs to be fixed, mitral regurgitation.
You mentioned something that’s near and dear to my heart, though. People see their reports. One of the things that is a little bit of a thorn in my side with respect to the way we manage health is that we have these fabulous studies that give us all this data, left atrial dimensions, pulmonary artery pressures, tricuspid insufficiency, mitral insufficiency, ventricular chamber dimensions, strain, circumferential and longitudinal strain, these subtle ways of looking at heart muscle performance.
Unfortunately, often, people just get the echo and say, oh, yeah, your mitral regurgitation looks about the same. It’s important that if the patient sees a number that’s out of balance or that it’s changed, it’s important they have an answer. Why is it different? Why is my left atrium larger now? Why does this suggest that my pulmonary artery pressures are higher? I know my mitral valve looks the same, but is it worrisome that I have more leak in my tricuspid valve? Now, a lot of the times, it’s not going to be anything. It’ll be a variation in their volume status or whatever, but often, it is a little step towards pathology. I think people have to be their own advocates because doctors are looking at a lot of things, a lot of reports, and sometimes they don’t have time to really ferret through those details. You shouldn’t be afraid to ask those questions.
Adam Pick: Dr. Gerdisch, I love the fact that you brought up the use of the word advocacy for patients. Because we need to know our bodies. We need to know our hearts. We need to know the changes that can happen with a disease as insidious as heart valve disease overtime. On behalf of all the patients in our community, thank you so much for these wonderful words of advice and insights about the need for mitral valve surgery.