Rigid Sternal Fixation: A New Approach to Sternal Closure
Written By: Allison DeMajistre, BSN, RN, CCRN
Medical Expert: Marc Gerdisch, MD, Chief of Cardiac Surgery, Franciscan Health, Indianapolis
Reviewed By: Adam Pick, Patient Advocate, Author & Website Founder
Page Last Updated: September 2, 2024
To access and fix your heart during an operation, your surgeon may cut your sternum, also called a sternotomy. When the procedure is complete, most surgeons typically use stainless steel wires to hold your sternum back together as the bone heals. The wire will stay in your sternum forever and your bones will heal around the wire.
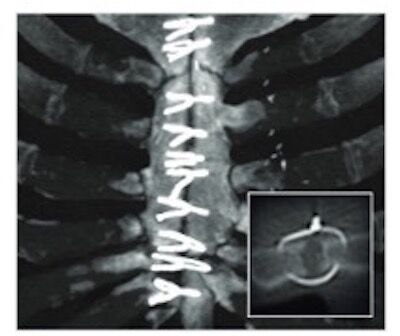 Sternal Wires
Sternal Wires
After surgery, you will be under strict sternal precautions as it typically takes up to eight weeks for your sternum to heal. During the healing process, you won’t be able to pull or push anything heavier than five pounds, use your arms to push yourself up from a sitting position or drive until cleared by your surgeon.
However, there is another way to close the sternum that offers a faster recovery time and minimal pain. The technique is called Rigid Sternal Fixation. Although orthopedic surgeons have used Rigid Sternal Fixation for years, cardiac surgeons continue to be slow in adopting it.
 Rigid Sternal Fixation
Rigid Sternal Fixation
To this point, we received a great patient question from Brad, who had heard of Rigid Sternal Fixation and asked us, “How many centers of excellence now use Rigid Sternal Fixation systems versus the old way of just using wire to close a sternotomy?”
To answer Brad’s question, we met with Dr. Marc Gerdisch during the Annual Meeting of The Society of Thoracic Surgeons in San Antonio, Texas. Dr. Gerdisch is the Chief of Cardiac Surgery at Franciscan Health in Indianapolis, Indiana. He also serves on the Advisory Board of the Enhanced Recovery After Cardiac Surgery (ERAS) Society, which lists Rigid Sternal Fixation as an expert recommendation for faster recovery after cardiac surgery.
Key Learnings About Rigid Sternal Fixation During Heart Valve Surgery
- Managing the sternum is part of the Enhanced Recovery After Surgery Program. “As many people know, I’m a little “evangelical” when it comes to how we manage a sternum and how we manage the perioperative experience,” said Dr. Gerdisch. “It’s all part of our Enhanced Recovery After Surgery program, which we really shouldn’t even call it ‘after surgery’ because we start before surgery.” He told us that when patients can’t have minimally invasive surgery with an incision between the ribs, the sternum will need to be repaired. Proper sternal management is an essential component of ERAS.
- Nationally, only five percent of cardiothoracic (CT) surgeons use rigid sternal fixation. “The only medical discipline that doesn’t repair a bone orthopedically after they divide it, or when they treat a bone, is cardiothoracic surgery,” Dr. Gerdisch said. “Now, for the last several years, we have done rigid plate fixation. In other words, we’ve done an orthopedic repair for every sternum we’ve split. We’ve benefitted from that and, in the process, have accelerated the recovery and delivered that message.” He said that although there has been some increase, only about five percent of CT surgeons in the United States use Rigid Sternal Fixation. At Franciscan Health, they use it 100 percent of the time. “Someone may ask, ‘Why is that?’ I don’t have a great explanation,” said Dr. Gerdisch. “But I’ll try to explain some of it.”
- The goal is to reduce the discomfort and limits on mobility after surgery. Gerdisch said their goal is to reduce the disability that comes from the operation. “Surgery is traumatic,” he said. “There’s some price that we pay as human beings when we have surgery, whether it’s discomfort, limitation of mobility, etc. Our focus was to condense that. For example, our patients are allowed to drive right away, lift things right away, use their arms to get up out of bed, get up off the toilet, and do all the normal things.”
- Repairing the sternum the old way didn’t make sense anymore. Gerdisch told us patients can’t return to regular activity if their sternum is delicate and moveable. “For 70 years, surgeons have been putting the bone together like a coat hanger, twisting it with a piece of wire,” he said. “We just thought that didn’t make sense anymore. Now we have a situation where most people can go completely back to their normal activity very, very soon after surgery.” He said that many people may wonder why everybody doesn’t do it this way, and the only reason he can come up with is that it costs money.
- Regarding cost, it’s more important to look at how patients will be in the long term rather than just 30 days after surgery. “It does cost money, but we’ve shown that it becomes cost neutral within about 60 days and probably upside within about 90 days if we include the fact that patients don’t have to go to extended care facilities and the incidents of complications related to the wound go down,” Dr. Gerdisch said. “Any time there’s a complication related to the wound, it’s very expensive. Unfortunately, our healthcare system is based on a 30-day pay structure. You really have to have an institution that gravitates towards looking at the long game. What is the experience for the patient going to be after they leave the hospital? How are they going to be in 90 days, a year, two years, three years?”
- Using Rigid Sternal Fixation takes more time in the operating room, which some surgeons don’t like. Gerdisch explained that time is another factor because the way they do Rigid Sternal Fixation now takes extra time at the end of the operation. “We have to conform titanium plates to the surface structure of the bone and fix those in place after we’ve brought the bone together,” he said. “Right now, we’re working on more advanced methods of everything, how we can bring the bone together faster, better, more compactly so that other surgeons feel a little bit more comfortable with their closure.” He said that some surgeons aren’t comfortable with the amount of time Rigid Sternal Fixation takes, so they are now working on creating plate fixation methods that don’t require as much of an investment of time at the end of surgery. “It doesn’t take an hour,” he said. “It takes an extra 15 minutes, but they feel like that’s an issue.” Dr. Gerdisch believes time and money are the two main issues holding most CT surgeons back from regularly using Rigid Sternal Fixation at the end of cardiac surgery.
Follow-Up Question #1: How Much Surgeon Experience is Needed for Rigid Sternal Fixation?
After watching Dr. Gerdisch’s video, I received an excellent question from Alex who asked, “How much experience should you look for with rigid sternal fixation in a cardiothoracic surgeon? As in, is it just as important to work with a high volume center as for a Ross Procedure? Or is it a simple enough method that low volume centers or less experienced teams could still see improved results over traditional closure mechanisms?”
Dr. Gerdisch responded, “Sternal fixation techniques are not complicated and can be performed well by most cardiac surgeons. It does benefit from having a surgeon who understands the orthopedic principles involved and is willing to invest the time and attention to detail to achieve optimal outcomes. Furthermore, it represents a component of an enhanced recovery after cardiac surgery (ERAS) program. Rigid fixation definitely has merit on it own in the same way as minimally invasive surgery, but for us, its value cannot be measured separately from the overall enhanced recovery program.”
Follow-Up Question #2: Can You See or Feel the Plates?
Here is another great, follow-up question from Ruth about rigid sternal fixation. Ruth asked me, “Does the rigid sternal fixation cause a “ridge” that is a raised part up from sternum? Would you see/feel it from outside?
Dr. Gerdisch responded, “The plates are very low profile in comparison to wires. Wires can create lumps or protrude, but we do still use them for the initial approximation of the two halves of bone. For patients who are very thin though, we do not use wires at all, and instead approximate the bone with FiberTapes prior to rigid fixation with plates. The FiberTapes have soft knots that can be tucked down alongside the sternum to avoid the protrusions created by wires, and the plates may be placed over them. The plates do have a shape and need to be properly contoured to the bone. Like any part of an operation, they need to be implanted with proper attention to detail. When well implanted, they are very difficult to detect and are really only appreciable to touch in people with very little soft tissue between the skin and plates.”
Follow-Up Question #3: Are Reoperations More Complicated?
Another excellent follow-up question from Ruth is, “Is it better/worse/same/more complicated to remove for subsequent surgeries? I would assume they just cut the old wires off during subsequent surgeries.”
Dr. Gerdisch responded, “For subsequent surgeries, the screws are removed (unscrewed) and the plates lift out. If for some reason rapid entry into the chest is needed, the cross bars of the plates can be rapidly cut and the plates split leaving half on each side of the sternum. They can later be removed if desired. As for better or worse, it takes a few minutes to take out the plates, but it is not difficult. In fact, taking out in-grown wires can be more challenging.”
Thanks Dr. Gerdisch and Franciscan Health!
On behalf of Brad and our entire HeartValveSurgery.com community, thank you, Dr. Gerdisch, for being ‘evangelical’ in this situation and working hard to spread the word on how surgeons can relieve the pain and reduce downtime for heart valve surgery patients. We also want to thank the team at Franciscan Health for taking great care of our heart valve patients!
- Doctor Q&A: Rapid Recovery Protocol 2.0
- Medical Advance: In-Operating Room Ventilator Removal
- Rigid Sternal Fixation: Top 6 Facts for Patients
Keep on tickin!
Adam
P.S. For the deaf and hard-of-hearing members of our patient community, I have provided a transcript of this interview with Dr. Gerdisch below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with heartvalvesurgery.com. We’re in San Antonio, Texas at the annual meeting of The Society of Thoracic Surgeons. I am thrilled to be joined by Dr. Marc Gerdisch who is the chief of cardiac surgery at Franciscan Health in Indianapolis, Indiana. Dr. Gerdisch, it is great to see you again and thanks for being with me today.
Dr. Gerdisch: Thanks, Adam.
Adam Pick: Yeah, so great meeting, learning a lot, and at the same time, we’re getting questions from patients. This one came in from Brad. It’s all about something you specialize in, which is recovery protocols. Brad asks, “How many centers of excellence now use rigid sternum closure systems versus the old way of using just wire to close a sternotomy?”
Dr. Gerdisch: That’s a really good question. As many people know, I’m a little evangelical when it comes to how we manage a sternum and actually how we manage the perioperative experience. It’s all part of our enhanced recovery after surgery program, which really we shouldn’t even call it after surgery because we start before surgery, but a really important pillar or component to that is how we manage the sternum. For the patients that we can’t do minimally invasive surgery for, patients that we can’t operate between the ribs, we have to divide the bone. Now we have a bone that needs to be repaired.
The only medical discipline that doesn’t repair a bone orthopedically after they divide it, or when they treat a bone, for some reason is cardiothoracic surgery. Now, we, for the last several years, have done rigid plate fixation. In other words, we’ve done an orthopedic repair for every sternum that we’ve split. We’ve really benefitted from that, and in the process, have accelerated the recovery. We have delivered that message. There’s been some increase nationally in the use but it’s out of about all the sterna that get put back together, it’s only out of about 5%. That’s 100% for us, about 5% nationally. Someone says, “Why is that?” I don’t have a great explanation, but I’ll try to explain some of it.
First of all, for us, our goal was to really condense the patient experience so that when they have heart surgery, no matter what the approach, the time out of their life, the disability that comes from the operation because surgery is traumatic and there’s some price that we pay as a human being when we have surgery, any surgery, pays some price, whether it’s discomfort, limitation of mobility, etc. Our focus was to eliminate – but you cannot really condense that and eliminate it. For example, our patients are allowed to drive right away, they can lift things right away, they can use their arms to get up out of bed, up out of the toilet, do all the normal things.
You can’t achieve that if the bone has to be addressed as something delicate that is moveable. For 70 years, surgeons have been putting the bone together basically like a coat hanger, twisting it with a piece of wire putting the bone together. We just thought that that just didn’t make any sense anymore. Now we’ve actually continued to advance the principles that we use. Now we have a situation where most people we can let them go completely back to their normal activity very, very soon after surgery. You would say, “Well, why doesn’t everybody do it?” The only things that I can really come up with are: folks talk about the fact that it costs money.
It does cost money, but we’ve shown that it becomes cost neutral within about 60 days and probably upside within about 90 days, if we include the fact that patients don’t have to go to extended care facilities and the incidents to complication related to the wound go down. Any time there’s a complicated related to the wound, it’s very expensive. Unfortunately, our healthcare system is based off of a 30-day pay structure. You really have to have an institution that gravitates towards looking at the long game. What is the experience for the patient going to be after they leave the hospital? How are they going to be in 90 days, a year, two years, three years?
The other is time. At the end of the operation, the way we do it, it takes time. We have to conform titanium plates to the surface structure of the bone and fix those in place after we’ve brought the bone together. Right now we’re working on more advanced methods of everything, how we can bring the bone together faster, better, more compactly so that other surgeons might feel a little bit more comfortable with their closure, and then are there methods of creating plate fixation that might not be as quite the investment of time that we make because for some reason surgeons are uncomfortable with that. It doesn’t take an hour. It takes an extra 15 minutes, but they feel like that’s an issue. Those are the two main issues that I can come up with.
Adam Pick: Yeah, well, Dr. Gerdisch, thank you so much for being evangelical in this situation because I’ve talked to your patients who’ve had rigid sternal fixation and there’s very little pain that they ever talk to me about. I’m sure this wraps into the whole decrease of opioid usage at Franciscan Health. On behalf of your patients and the people at heartvalvesurgery.com, thanks for everything you are doing at Franciscan Health in Indianapolis, Indiana.
Dr. Gerdisch: Thanks, Adam.