Surgeon Q&A: “Can The Ventilator Tube Be Removed Before I Wake Up in the Intensive Care Unit?” asks Joe
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: Dr. Marc Gerdisch, Chief of Cardiac Surgery, Franciscan Health
Published: April 28, 2024
Preparation for heart valve surgery is often extensive. Pre-surgery testing with blood work, chest x-rays, ultrasounds, and EKGs are just the beginning. You’ll likely meet with the surgeon and surgical team members so they can explain the entire process, from the day of surgery to what to expect once you arrive home.

Even with the best of information, one aspect of valve surgery many patients struggle with is waking up in the intensive care unit (ICU) with the breathing tube still in their throat. The first inclination is to reach for the tube to pull it out, sometimes in a panic, only to find their hands are tied down to prevent them from doing so. They are in unfamiliar surroundings with machines beeping and people they don’t know. Most patients, if given the choice, would prefer to have the breathing tube taken out in the operating room while they’re still asleep before being transferred to the intensive care unit for continuing care.
Although 24-hour ventilator times remain the quality metric for the Society of Thoracic Surgeons star-rating, surgeons are working hard to reduce ventilator times even more. Many leading cardiac centers specializing in heart valve procedures and replacements are adopting the Enhanced Recovery After Surgery (ERAS) approach. The idea is to use evidence-based practices to improve surgical care and recovery for better patient outcomes, and early extubation in the operating room is one of those approaches. Although ERAS has been applied to other types of surgeries for many years, its application to cardiac surgery is relatively new.
Advances for In-Operating Room Ventilator Tube Removal
We recently received a patient question from Joe on this topic. He asked, “I have been diagnosed with bicuspid aortic stenosis and will be undergoing surgical aortic valve replacement. Is it possible to have the ventilator tube removed before waking up in the ICU as I would like to avoid this process if possible?”
I met with Dr. Marc Gerdisch, the Chief of Cardiac Surgery at Franciscan Health in Indianapolis, Indiana, to answer Joe’s question. Dr. Gerdisch has performed thousands of cardiac surgeries and serves on the ERAS Advisory Board, making him the perfect match for Joe’s question.
Key Learnings About Early Extubation After Heart Valve Surgery
- The most important aspect of early extubation is safety. Dr. Gerdisch said that if everything is safe, the mechanics of ventilation are good. The patient is stable; they work hard to take the breathing tube out in the operating room while patients are still asleep so they don’t have to wake up in the ICU with the tube still in their mouth. “We’ve worked hard on that, the first end of it being what I said first, which is safe,” he said. “Can it be done safely? Is there a reason that the tube has to stay in? As it turns out, by virtue of multimodal effort to decrease the trauma around surgery and decrease the discomfort, we have achieved a very high rate of in-operating room extubations.”
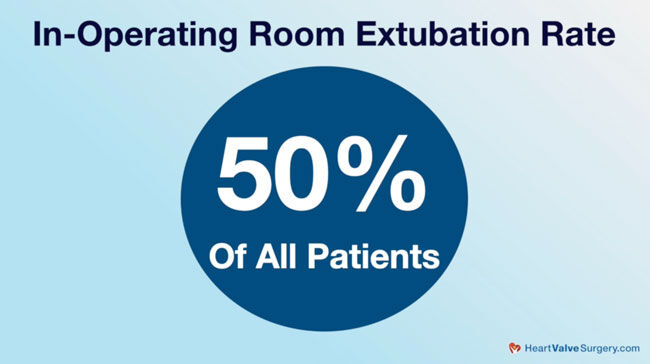
- The rate of early extubation depends on the patient and the type of surgery. Dr. Gerdisch told us that in their program, they are currently at 50% for early extubations, but that number includes sick patients who may be having a third reoperation or multi-valve operations. “When we look at the folks who are a little bit more straightforward, we get closer to 70% and 80% of those folks having the tube taken out in the operating room,” he said. “First, for minimally invasive patients, it’s nearly 100%. For sternotomy patients, though, we’re still pushing over 50% for a lot of those categories of patients.” Dr. Gerdisch believes they’ve achieved that number because they do rigid sternal fixation with sternotomy patients. “Then patients are comfortable, and their breathing mechanics are immediately good,” he said. “Minimally invasive, same thing, we use special methods to address discomfort, and as a result, people are comfortable and breathing mechanics are immediately good.”
- Bleeding is another aspect when deciding on early extubation. Dr. Gerdisch said, “Second question: is there any bleeding? We actually use a specialized type of chest tube. It’s an active clearance chest tube. This is something that, as a program, we had to decide if we wanted to invest in because there’s added expense there.” He told us that after a yearlong study looking at the impact of using the active clearance chest tube, they had a statistically significant decrease in transfusion rates. “There was already a very low transfusion rate,” said Dr. Gerdisch. “We lowered it even more.” When patients don’t have bleeding and are unlikely to need blood products, it means knowing the patient is stable. “Hemodynamically, they look good,” he said. “Patient’s comfortable. We know that there’s no bleeding. Take the tube out.”
Thanks Dr. Gerdisch and the Franciscan Health team!
On behalf of Joe and our entire patient community, many thanks to Dr. Gerdisch, for investing in the people, the processes, and the technology at Franciscan Health in Indianapolis, Indiana to accelerate the removal of the breathing tube in the operating room!
Related Links:
- Rapid Recovery Protocol 2.0: What Should Heart Surgery Patients Know?
- Dr. Marc Gerdisch Q&A: Restarting the Heart After Heart Surgery
Keep on tickin!
Adam
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with heartvalvesurgery.com. We’re in San Antonio, Texas at the annual meeting of The Society of Thoracic Surgeons. I am thrilled to be joined by Dr. Marc Gerdisch who is the chief of cardiac surgery at Franciscan Health in Indianapolis, Indiana. Dr. Gerdisch, it is great to see you again and thanks for being with me.
Dr. Gerdisch: Thanks, Adam.
Adam Pick: Yeah, so we are at STS, great meetings, presentations going on, and we’re getting a lot of questions from patients for experts like you. One of the questions is right in your specialty in terms of enhanced recovery after surgery, ERAS, and it comes in from Joe. He asks, “I have been diagnosed with bicuspid aortic stenosis and will be undergoing surgical aortic valve replacement. Is it possible to have the ventilator tube removed prior to waking up in the ICU as I would like to avoid this process if possible?”
Dr. Gerdisch: Yeah, this is a really good question because I feel the same way that he does, right? I think that, given the opportunity, if everything is safe, if the mechanics of my ventilation are good, if I’m stable, can the tube come out in the operating room while I’m still asleep and then I just come out to the floor in the unit without that tube and have to wake up with it in my mouth? We’ve worked hard on that, the first end of it being what I said first, which is safe. Can it be done safely? Is there a reason that tube has to stay in? As it turns out, by virtue of a multimodal effort to decrease the trauma around surgery and decrease the discomfort, we have achieved a very high rate of in operating room extubation.
Right now, for our program, it’s 50%, but that includes also some very sick people who might be having their third time reoperation, multivalve operation, but when we look at the folks who are a little bit more straightforward, we get closer to 70%, 80% of those folks having the tube taken out in the operating room. First, for minimally invasive, minimally invasive patients, it’s nearly 100%. For sternotomy patients, though, still we’re pushing over 50% for a lot of those category of patients. How did we achieve that? Folks know that we do rigid sternal fixation. If you have to have a sternotomy, the bone has to be split, then patients are comfortable and their breathing mechanics are immediately good.
Minimally invasive, same things, we use special methods to address discomfort, and as a result, people are comfortable, breathing mechanics are immediately good. Second question: is there any bleeding? They just had heart surgery. We actually use a specialized type of chest tube. It’s an active clearance chest tube. This is something that as a program we had to decide if we wanted to invest in because there’s added expense there. We did a yearlong study to look at the impact of using those tubes. What we found was that we had a statistically significant decrease. There were already very low transfusion rate. We lowered it even more.
What we realized the reason was that in the operating room we’re so sure that we don’t have bleeding that we’re very unlikely to give any blood products. That translate then to we know the patient is stable. Hemodynamically, they look good. Patient’s comfortable. We know that there’s not bleeding. Take the tube out.
Adam Pick: Well, Dr. Gerdisch, as a patient who woke up in the intensive care unit with the ventilator tube still in, one, it was unexpected, and two, it was very uncomfortable, so I can’t thank you for taking the time to answer Joe’s question and investing in the people, the processes, and the technology at Franciscan Health in Indianapolis, Indiana. Thanks so much for being here today.
Dr. Gerdisch: Thanks.
Adam Pick: Hi, everybody. It’s Adam. I hope you enjoyed that video. Don’t forget you can always subscribe to our YouTube channel, watch the next two educational videos coming up on your screen, or click the blue button to visit heartvalvesurgery.com.
 Dr. Marc Gerdisch
Dr. Marc Gerdisch